Volume 11, Issue 2 (2025)
Pharm Biomed Res 2025, 11(2): 147-158 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zahir Mirdamadi N, Jamshidi H R, Moravej K, Aghazadeh-Habashi K, Rafatmagham S, Farnaghi F, et al . Clinical, Paraclinical, and Prognostic Findings of Iranian Patients Poisoned With Tricyclic Antidepressants: A Cross-sectional Study. Pharm Biomed Res 2025; 11 (2) :147-158
URL: http://pbr.mazums.ac.ir/article-1-662-en.html
URL: http://pbr.mazums.ac.ir/article-1-662-en.html
Negar Zahir Mirdamadi1 

 , Hamid Reza Jamshidi2
, Hamid Reza Jamshidi2 

 , Khashayar Moravej3
, Khashayar Moravej3 

 , Komeil Aghazadeh-Habashi4
, Komeil Aghazadeh-Habashi4 

 , Sareh Rafatmagham5
, Sareh Rafatmagham5 

 , Farhad Farnaghi1
, Farhad Farnaghi1 

 , Hamid Reza Ghasemirad2
, Hamid Reza Ghasemirad2 

 , Raheleh Kadivari6
, Raheleh Kadivari6 

 , Hamid Owliaey *7
, Hamid Owliaey *7 




 , Hamid Reza Jamshidi2
, Hamid Reza Jamshidi2 

 , Khashayar Moravej3
, Khashayar Moravej3 

 , Komeil Aghazadeh-Habashi4
, Komeil Aghazadeh-Habashi4 

 , Sareh Rafatmagham5
, Sareh Rafatmagham5 

 , Farhad Farnaghi1
, Farhad Farnaghi1 

 , Hamid Reza Ghasemirad2
, Hamid Reza Ghasemirad2 

 , Raheleh Kadivari6
, Raheleh Kadivari6 

 , Hamid Owliaey *7
, Hamid Owliaey *7 


1- Department of Toxicology, School of Pharmacy, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Student Research Committee, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Faculty of Dentistry, Isfahan Branch, Islamic Azad University, Isfahan, Iran.
4- Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran.
5- Department of Internal Medicine, Fasa University of Medical Sciences, Fasa, Iran.
6- Department of Medical Science, Faculty of Medicine, Yazd Branch, Islamic Azad University, Yazd, Iran.
7- Department of Forensic Medicine & Clinical Toxicology, Faculty of Medicine, Yazd Branch, Islamic Azad University, Yazd, Iran.
2- Student Research Committee, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Faculty of Dentistry, Isfahan Branch, Islamic Azad University, Isfahan, Iran.
4- Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran.
5- Department of Internal Medicine, Fasa University of Medical Sciences, Fasa, Iran.
6- Department of Medical Science, Faculty of Medicine, Yazd Branch, Islamic Azad University, Yazd, Iran.
7- Department of Forensic Medicine & Clinical Toxicology, Faculty of Medicine, Yazd Branch, Islamic Azad University, Yazd, Iran.
Keywords: TCA poisoning, Tricyclic Antidepressant (TCA) poisoning, Prognosis suicide, Attempts nortriptyline poisoning
Full-Text [PDF 646 kb]
(402 Downloads)
| Abstract (HTML) (919 Views)
Full-Text: (318 Views)
Introduction
Depression is a debilitating, financially burdensome, and lethal disorder [1-4]. Currently, the treatment of depression is carried out by specialists through a combination of psychotherapy, pharmacological therapy, electroshock, and lifestyle modifications, and the beneficial effects of these strategies are mainly synergistic [2-4]. Pharmacological treatment is a key component in the treatment of depression, particularly in severe cases and circumstances that necessitate rapid intervention [2]. Tricyclic antidepressants (TCAs) are a class of pharmacological medications that are used in the treatment of major depressive disorder (MDD), nocturnal enuresis, and chronic pain [5, 6]. TCAs initially launched in the market in 1959 [7]. These medications exert their effect by blocking the reabsorption of neurotransmitters, like serotonin and norepinephrine, which can influence mood, focus, and pain perception in individuals [8].
TCA intoxication can happen in instances of suicide and accidental overdose. The consumption of TCAs could cause neurological complications, such as confusion, seizures, as well as cardiac issues, including tachycardia, QTc prolongation, widened QRS complex, and hypotension. Other adverse effects of TCAs include blurred vision, constipation, xerostomia, confusion, and urinary retention [8].
Considering the multiple complications related to TCA poisoning, as well as the availability of these drugs and their potential for abuse, this retrospective cross-sectional study aimed to investigate patients with TCA poisoning who were admitted to Shah Vali Hospital in Yazd, Iran, and Shahid Beheshti Taft Hospital in Taft, Yazd, Iran, between 2014 and 2023. The study also sought to evaluate the frequency of clinical, paraclinical, and prognostic findings in these patients.
Materials and Methods
Inclusion and exclusion criteria
This retrospective cross-sectional study included all poisoned patients with TCAs who were admitted to Shah Vali Hospital, Yazd, Iran, and Shahid Beheshti Hospital, Taft, Yazd, Iran, from 2013 to 2022. The medical history and clinical examination of the patients were consistent with the symptoms of TCA poisoning. Moreover, this study excluded patients poisoned with other agents or unknown agents, and patients with incomplete medical records.
Data collection
The medical records and the hospital information system (HIS) were reviewed to collect the demographic characteristics and clinical findings of poisoned patients with TCAs. The clinical findings included neurological findings, cardiovascular findings, paraclinical findings, therapeutic interventions, outcomes, and mortality of poisoned patients with TCAs.
The demographic characteristics included age, gender, marital status, education, hospitalization time, the cause of taking drugs, the history of abuse, the severity of the disease—in terms of hospitalization in the intensive care unit (ICU) or poisoning department—and rhabdomyolysis (CPK >975 IU/L).
The neurological findings included agitation, seizures, and pupillary mydriasis. Cardiovascular findings included fluctuating changes in blood pressure (BP), tachycardia, the morphology of the R wave in lead aVR, and QRS complex prolongation. Paraclinical findings included the levels of white blood cells (WBC), potassium (K), arterial blood gas/ venous blood gas (ABG/VBG), and blood pH. Therapeutic interventions included the administration of dopamine, sodium bicarbonate, norepinephrine, and intubation with a tracheal tube.
Statistical analysis
SPSS software, version 23 (SPSS Inc., Chicago, IL, USA) was utilized for statistical analysis. Qualitative variables were presented as frequencies (percentages). The statistical differences between groups were investigated by the chi-square and Fisher’s exact tests. All statistical analyses were conducted using a two-tailed approach. P<0.05 was considered statistically significant.
Results
This retrospective cross-sectional study included 233 poisoned patients with TCAs. Table 1 summarizes the demographic characteristics.
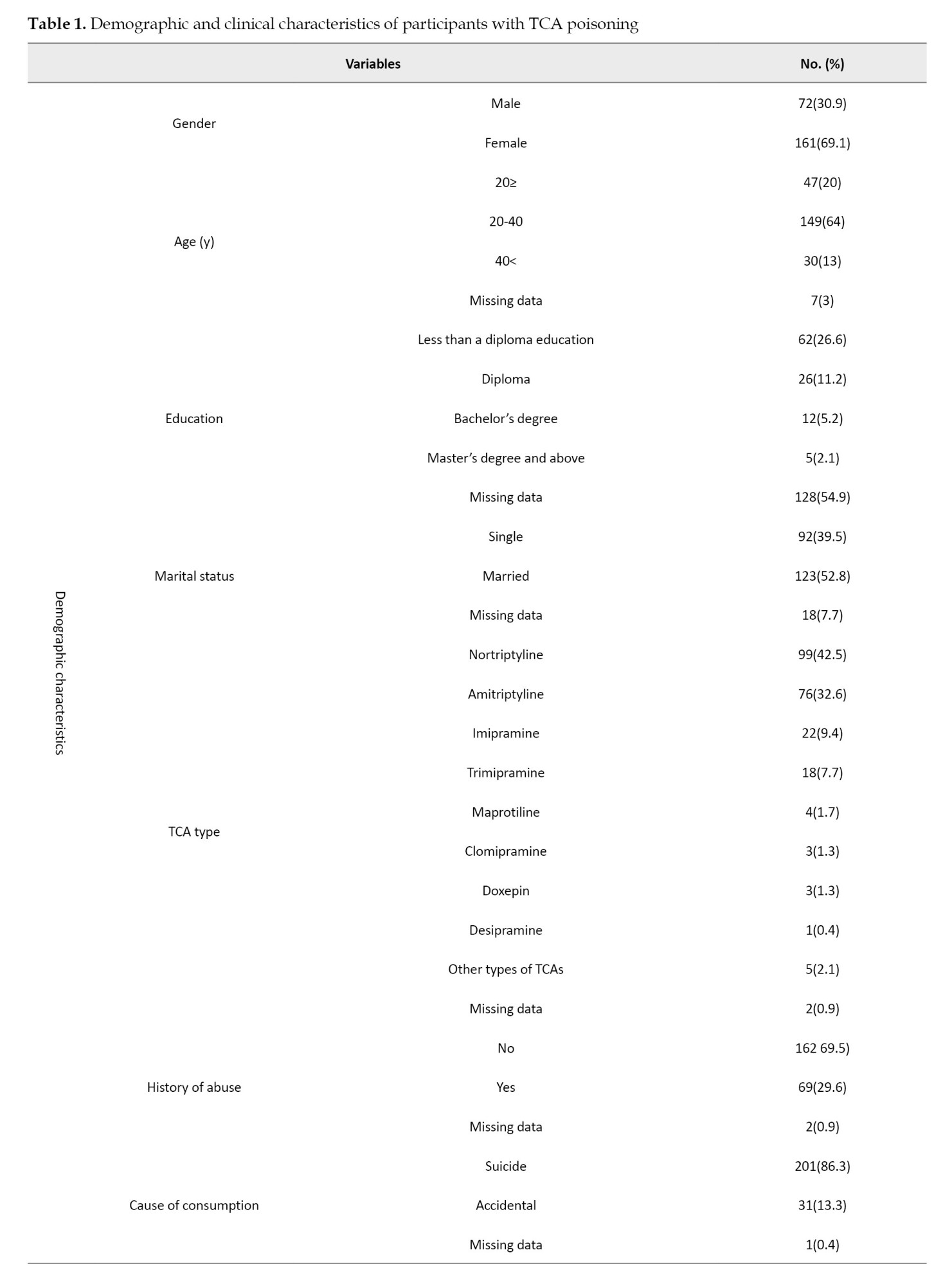
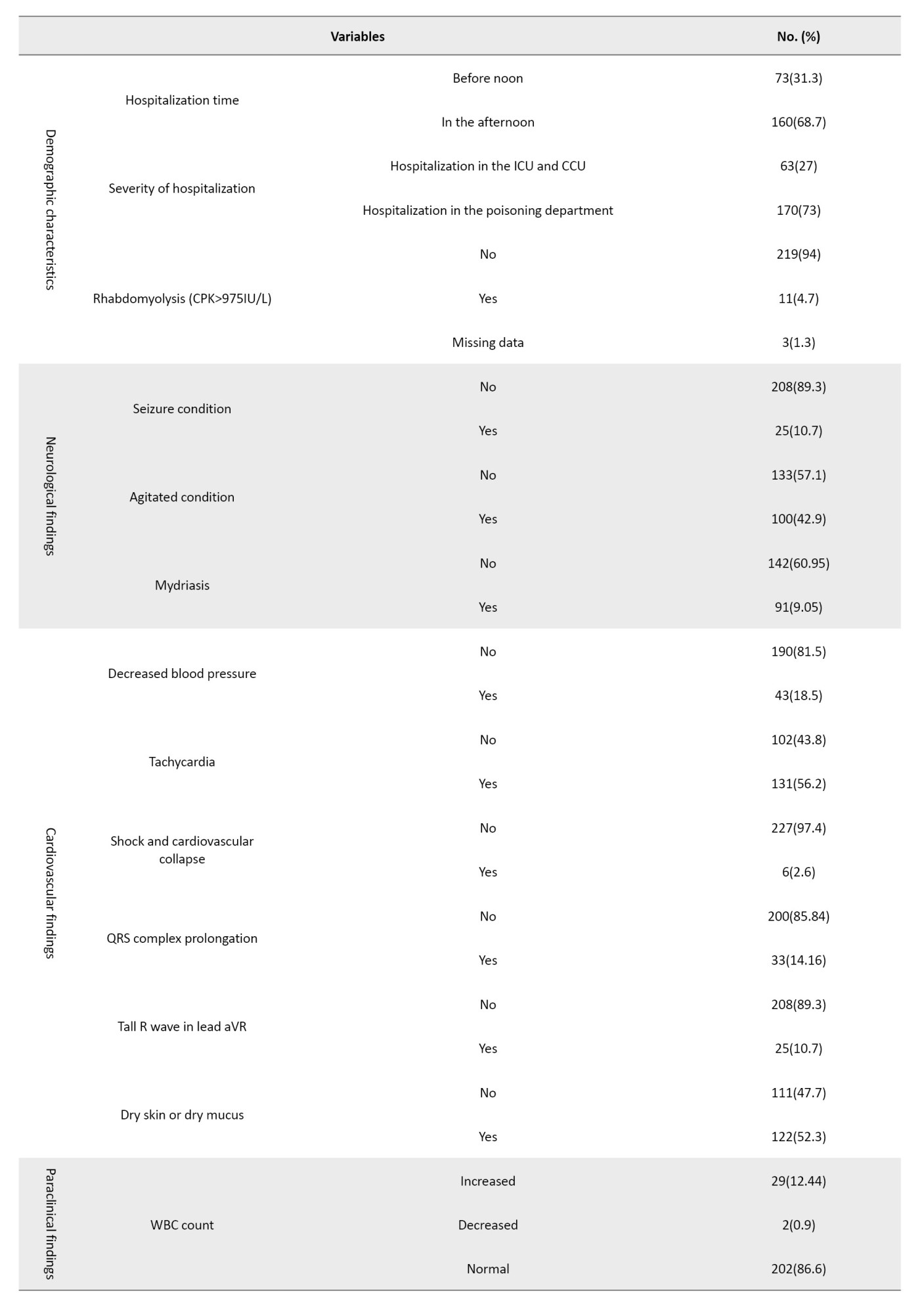
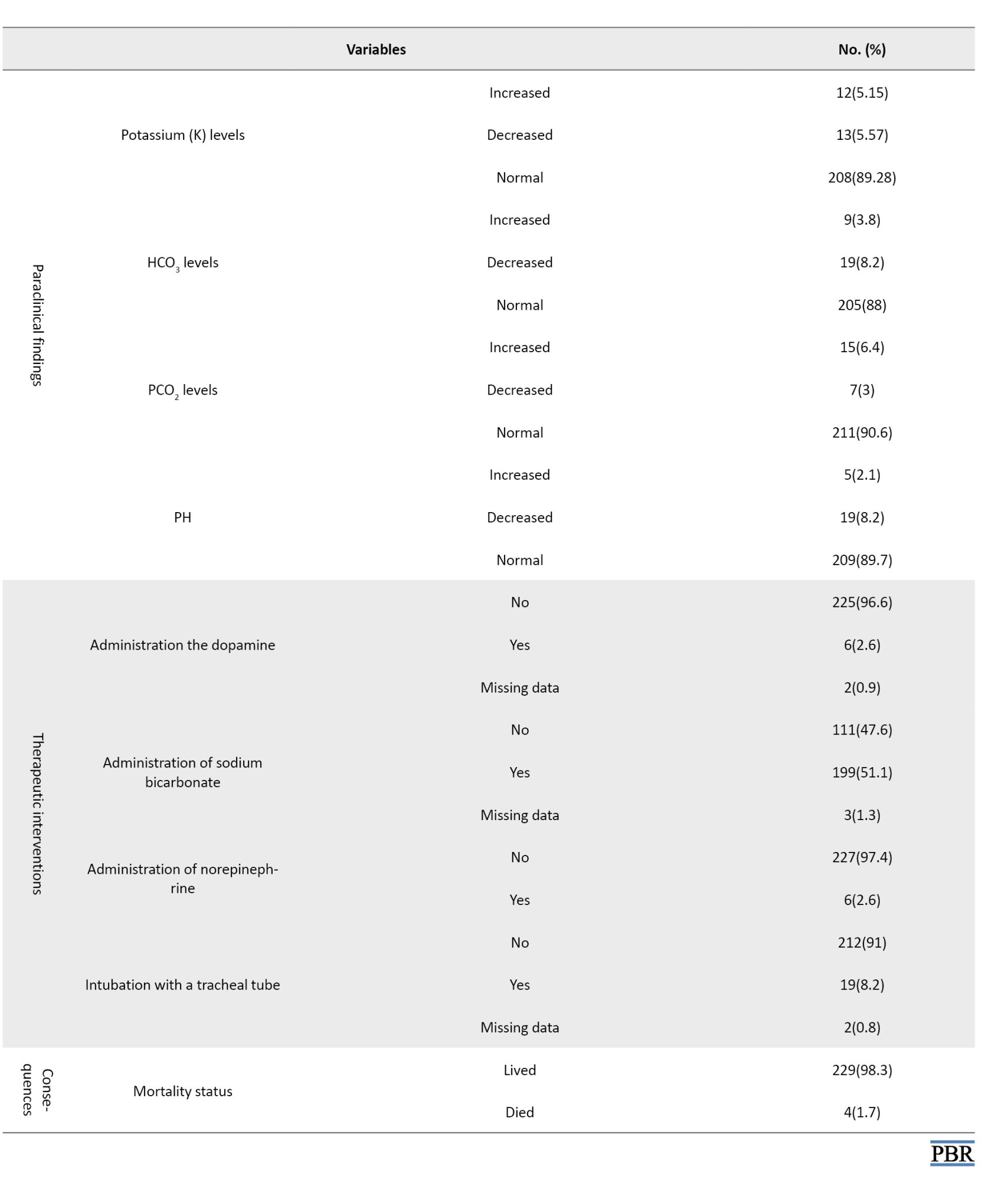
The most TCA-poisoned patients were female (69.1%). The age range of these patients was 2 to 67 years with a mean age of 28.11 years and the patients aged 20-40 years were more significantly impacted by TCA poisoning (64%). Analysis of the patient’s education and marital status showed that the highest frequency of TCA-poisoned patients was related to individuals with less than a diploma education (6.26%) and married individuals, comprising 52.8% of the cases. The most commonly reported TCAs were nortriptyline (42.5%) and amitriptyline (32.6%). Determining the frequency of previous abuse history among patients revealed that a history of previous abuse was seen in 29.6% of patients. The data indicated that the majority of patients had a history of suicide attempts (86.3%). Also, 68% of the patients were hospitalized during the afternoon. According to the results, 73% of the patients were hospitalized in the poisoning department. Rhabdomyolysis was identified in 4.7% of the patients. Seizures were observed in 10.7% of the individuals. The assessment of agitation frequency among patients revealed that agitation was present in 42.9% of the individuals. Mydriasis was observed in 39.05% of the patients.
A decrease in blood pressure was observed in 18.5% of the patients. Tachycardia was seen in 56.2% of cases. The shock was observed in 2.6% of the patients. QRS complex prolongation was observed in 14.16% of the patients. The results presented in Table 1 indicated that a tall R wave in the augmented vector right (aVR) lead was observed in 10.7% of the patients. Additionally, 52.3% of patients exhibited dry skin and mucous membranes. An increase and decrease in WBC count was observed in 12.44% and 0.9% of patients, respectively. The findings showed that increased and decreased potassium levels were observed in 5.15% and 5.57% of patients, respectively. Increases and decreases in HCO3 levels were observed in 3.8% and 8.2% of patients, respectively. Moreover, increases and decreases in PCO2 were found in 6.4% and 3%, respectively. As indicated, increased and decreased pH levels were observed in 2.1% and 8.2% of patients, respectively. The administration of dopamine, bicarbonate, and norepinephrine was noted in 2.6%, 51.1%, and 2.6% of the patients, respectively. Examining the frequency of patient mortality showed that 1.7% of patients died.
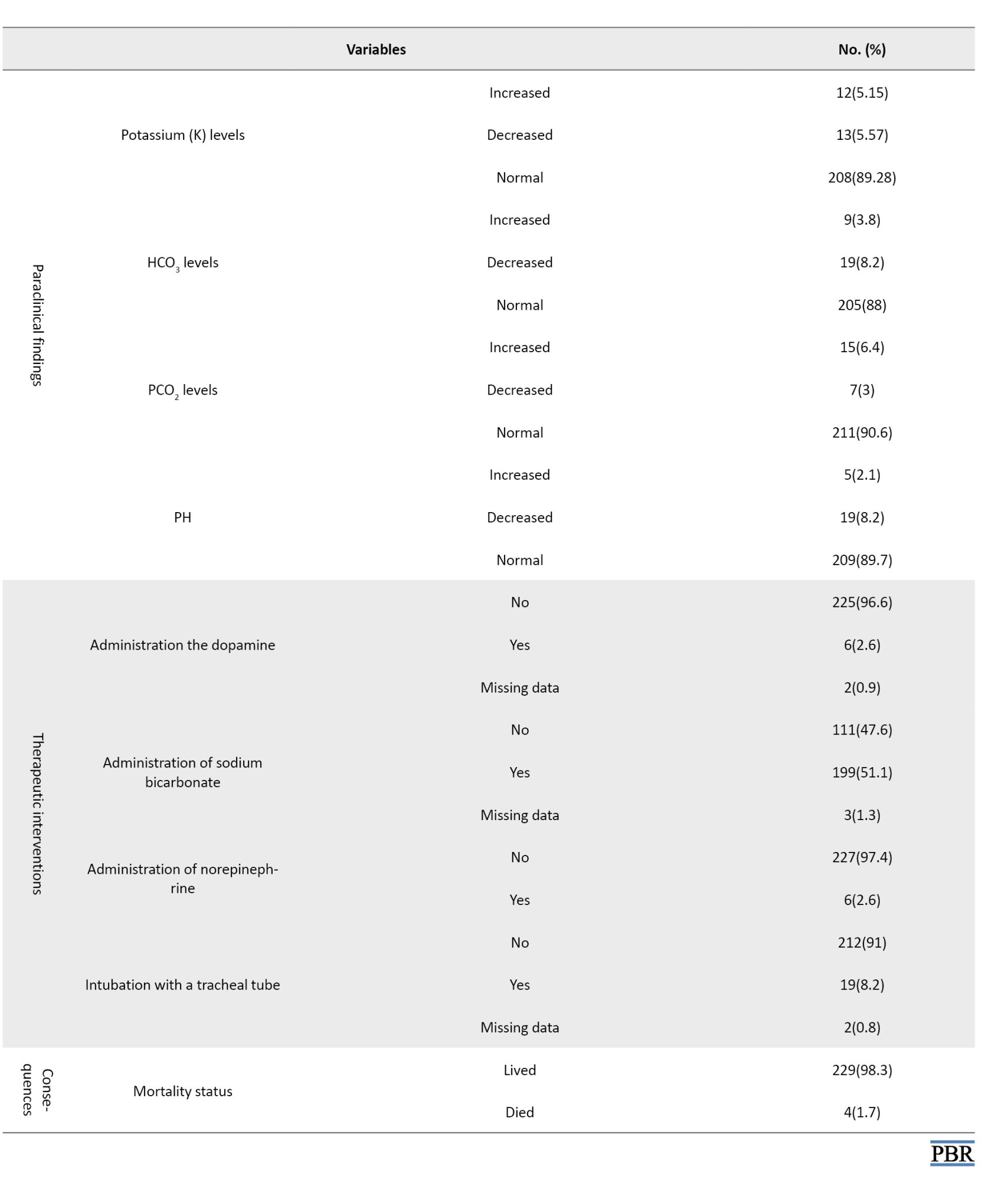
Table 2 presents a comparative analysis of the association between various demographic and other variables and the nine categories of TCAs.
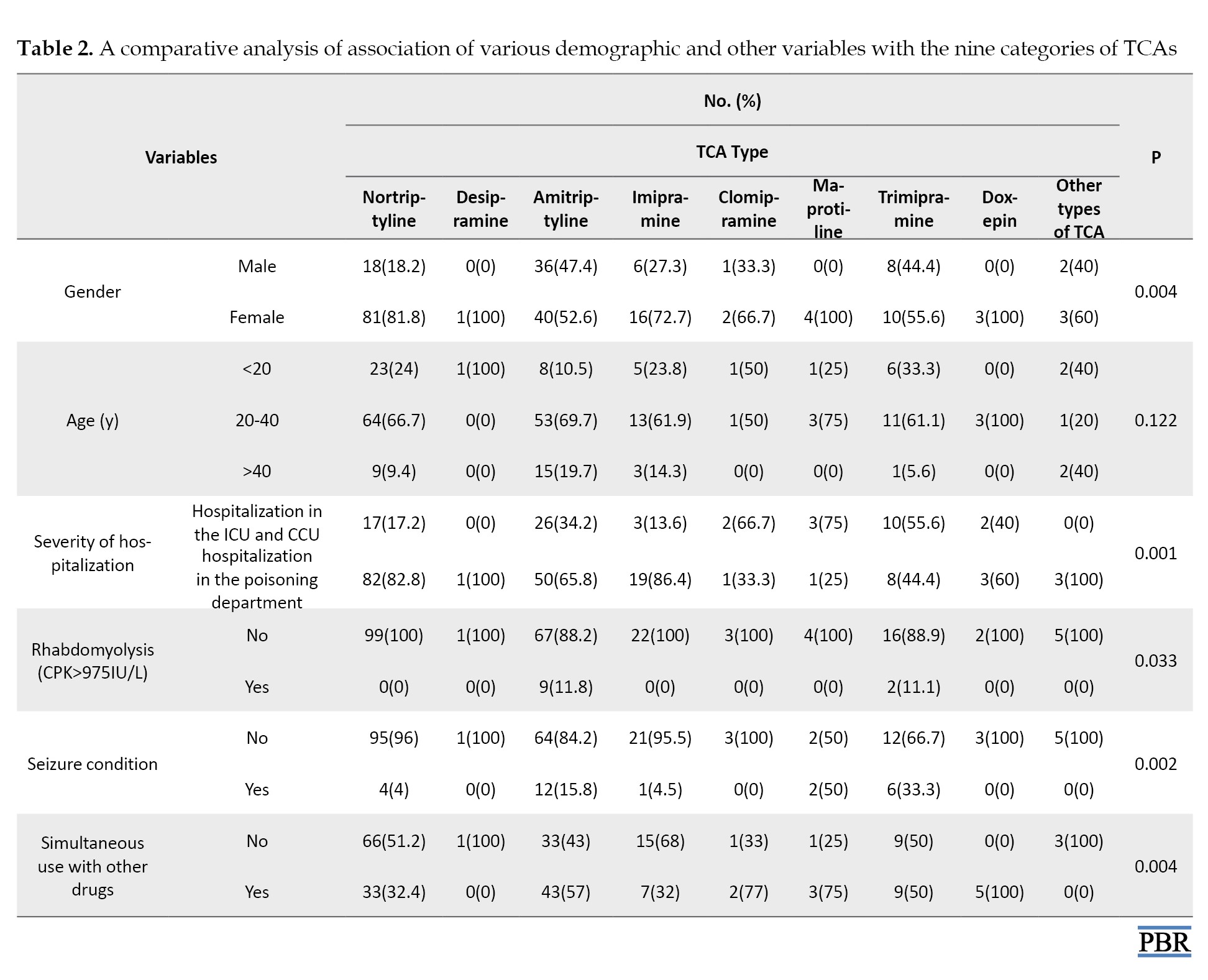
There was a notable relationship between TCA type and gender (P=0.004). Among the 160 women studied, 81(50.62%) were prescribed nortriptyline, whereas among the 71 men, 36(50.70%) were prescribed amitriptyline.
There was no significant difference between the TCA types and age (P=0.122). There was a significant relationship between TCA type and the severity of the disease (P=0.001). Specifically, among the 63 cases hospitalized in the ICU and CCU, amitriptyline was the most frequently prescribed, accounting for 26 cases (41.2%).
There was a significant relationship between the frequency of TCA types and the occurrence of rhabdomyolysis (P=0.033). Notably, among the 11 cases of rhabdomyolysis identified, 9 cases (81.81%) were associated with amitriptyline.
There was a significant relationship between the frequency of TCA types and the occurrence of seizures (P=0.002). Specifically, among the 25 individuals experiencing seizures, the highest frequency was associated with amitriptyline, accounting for 12 cases (48%).
There was a significant relationship between the TCA types and the method of drug administration (P=0.004). This suggests a noteworthy relationship between the type of TCA used and the manner of its administration. Notably, amitriptyline exhibited the highest frequency of concurrent drug use, accounting for 43 out of 102 cases (42.2%).
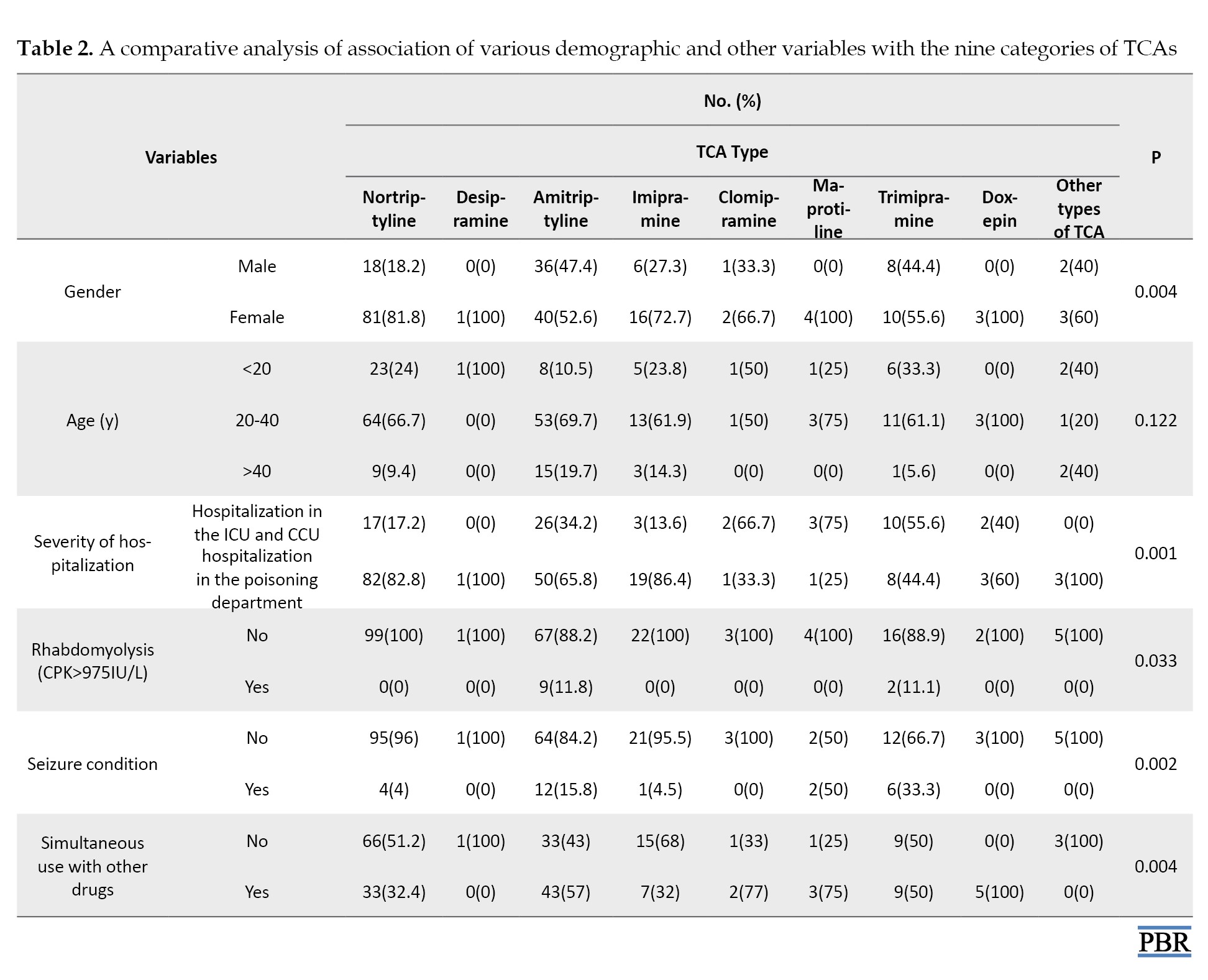
Table 3 presents a comparative analysis of the association between mortality and other variables.
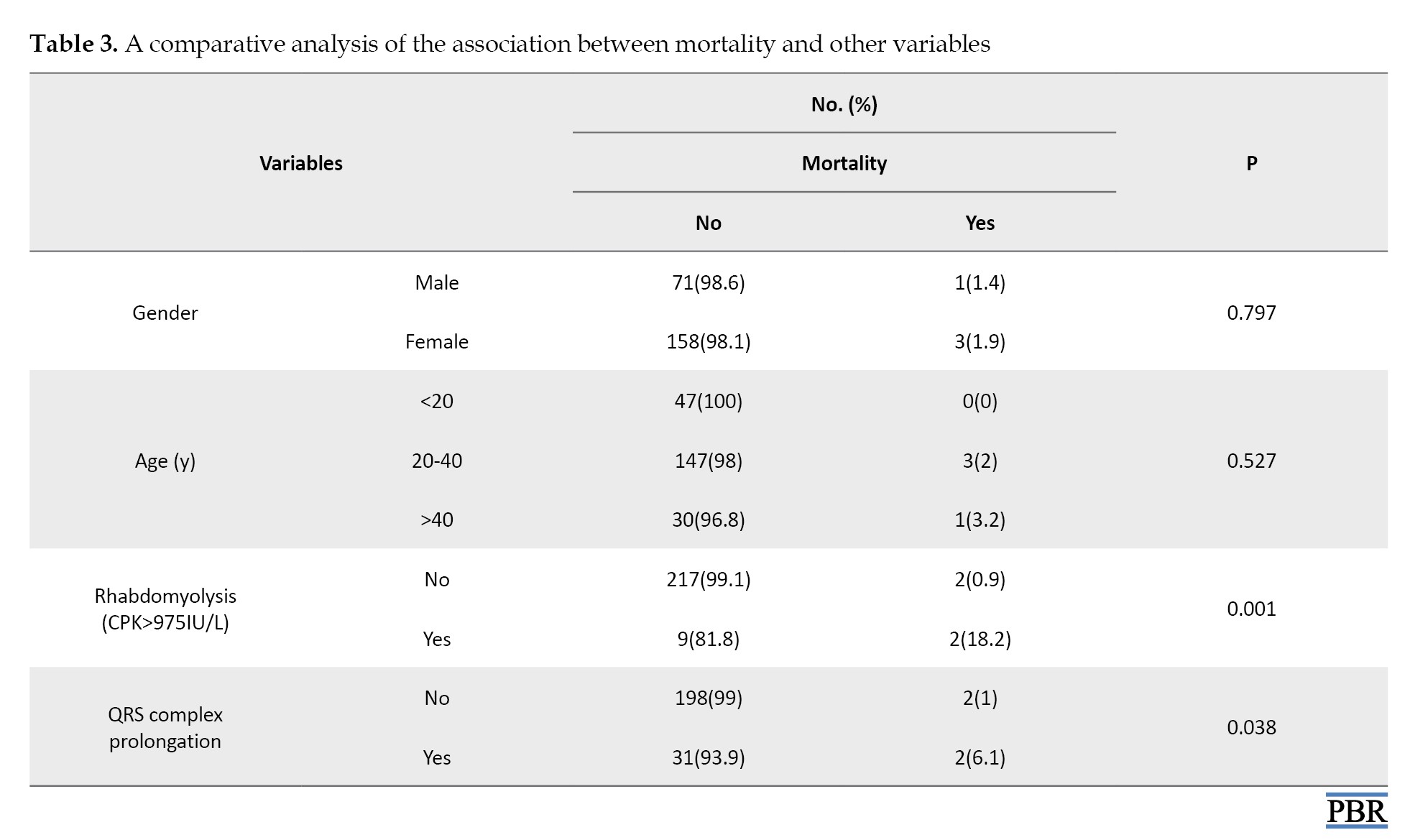
There was no association between the frequency of mortality and gender and age (P=0.797 and P=0.527, respectively). There was a significant association between the frequency of death and rhabdomyolysis (P=0.001). This suggests a meaningful relationship between mortality and the presence of rhabdomyolysis, with 2 out of 4 cases of death (50%) occurring in individuals with this condition. Additionally, the findings reveal a significant association between mortality and QRS complex prolongation (P=0.038). This indicates a significant relationship between mortality and QRS complex lengthening, with 2 out of 4 cases of death (50%) involving patients who exhibited QRS complex prolongation.
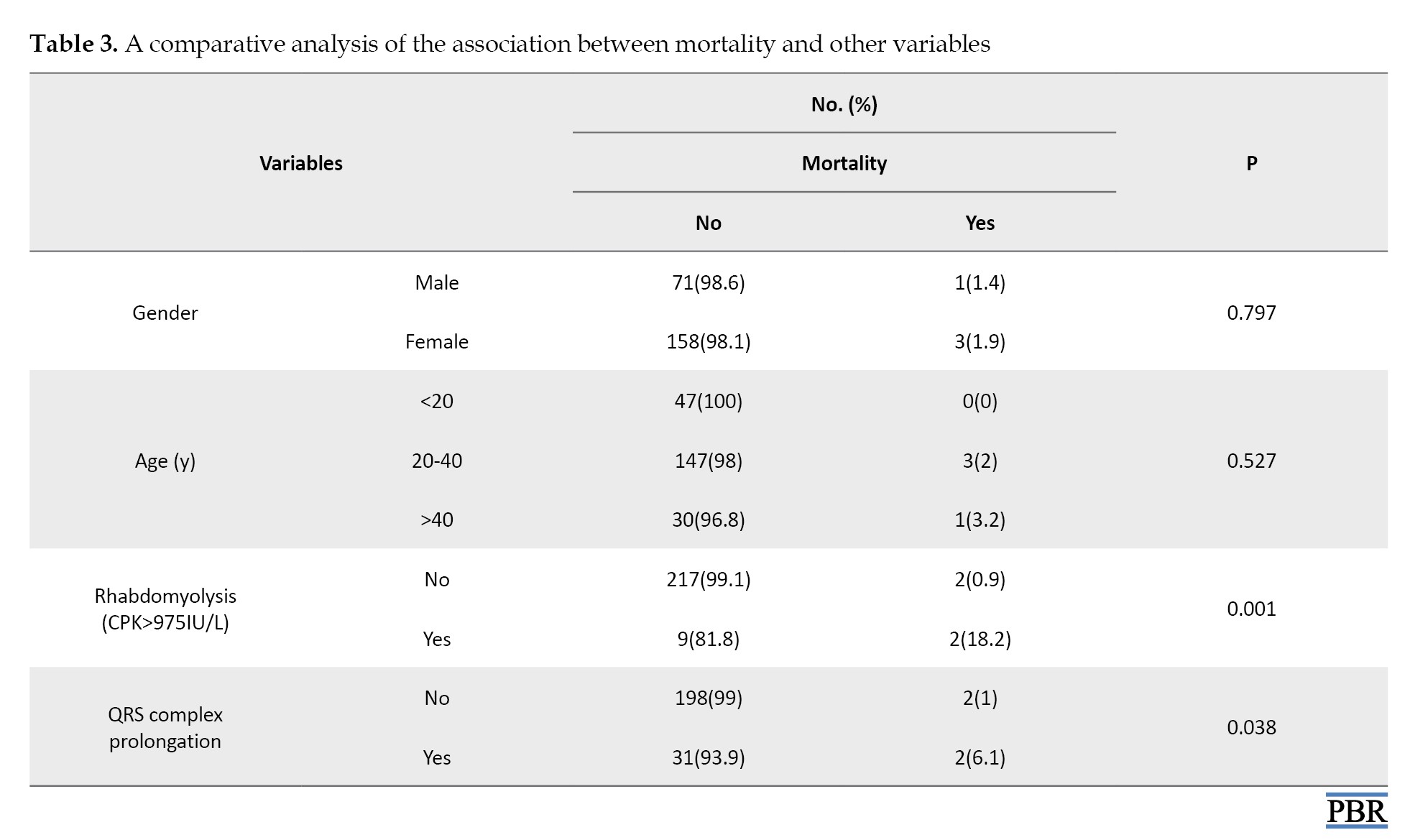
Table 4 presents a comparative analysis of the association between QRS complex prolongation and other variables.
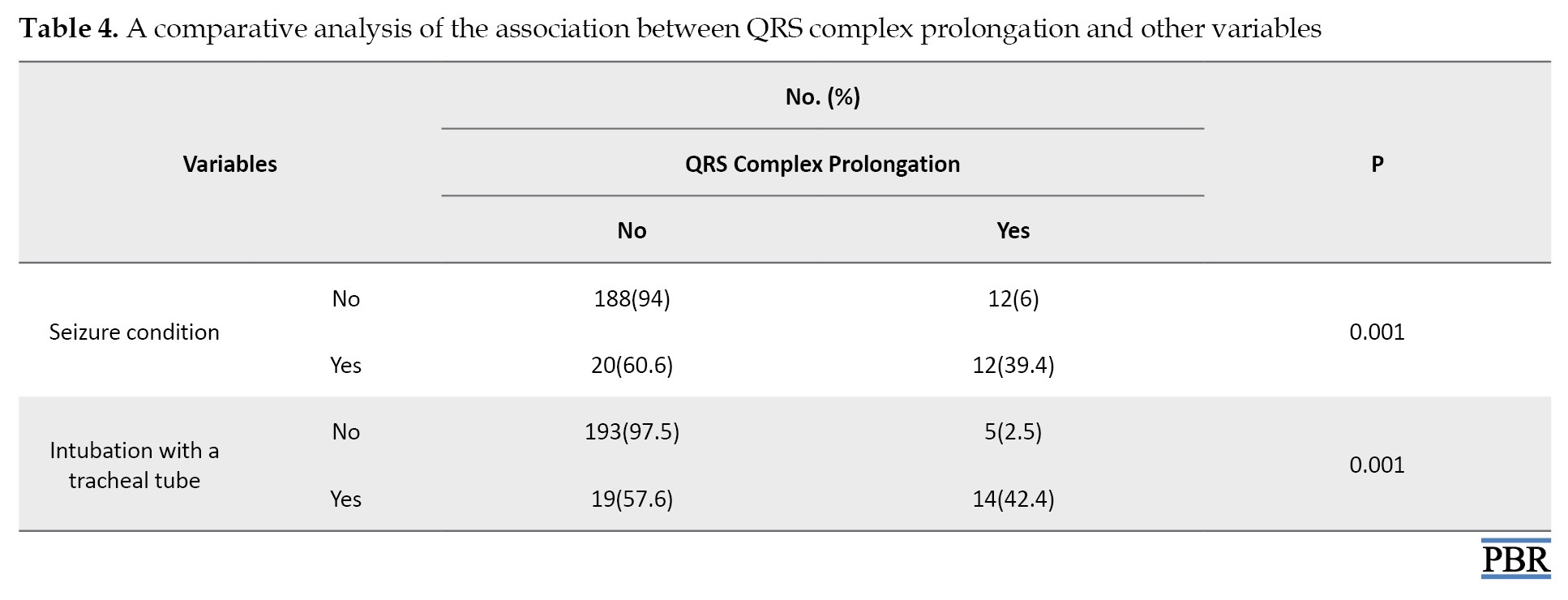
The findings in the table above revealed a significant association between the frequency of QRS complex lengthening and seizures (P=0.001). This suggests a noteworthy relationship between QRS complex prolongation and the occurrence of seizures, with 12 out of 32 cases of QRS complex prolongation (37.5%) involving patients who experienced seizures. Furthermore, the results indicated a significant association between the lengthening of the QRS complex and intubation with a tracheal tube (P=0.001). This finding highlights a significant relationship between QRS complex prolongation and tracheal intubation, as intubation was observed in 14 out of 33 cases of QRS complex prolongation (42.42%).
Discussion
This retrospective cross-sectional study investigated 233 TCA-poisoned patients with an age range of 2 to 67 years and with a mean age of 28.11 years between 2013 and 2022. Gheshlaghi et al. found 92 cases of TCA-poisoned patients with a mean age of 27.5 and an age range of 16–65 over two years [5]. In our study, similar to Saleh et al., the majority of patients were in the age group of 20-40 years [6]. These similarities indicate that TCA poisoning occurs more frequently in young and middle-aged groups. These findings suggest that young and middle-aged individuals, who may be at higher risk for various reasons such as depression or easy access to these drugs, constitute the majority of poisoning cases.
According to our findings, most of the TCA-poisoned patients were female (69.1%). Similarly, females predominated in other studies [5, 6]. The results of this study indicate that TCA toxicity was more common in women than in men.
Based on the patients’ education and marital status, people with less than a diploma education (26.6%) and married individuals (52.8%) comprised the highest frequency of TCA-poisoned patients. Based on Aslan et al.’s study, 47.5% of TCA-poisoned individuals were married, and 37% had less than a diploma education, respectively [9].
The majority of patients were poisoned with nortriptyline (42.5%) and amitriptyline (32.6%). Other studies align with our study [5, 6, 9]. Aslan et al. reported that the higher prevalence of amitriptyline poisoning can be attributed to the lower cost of this antidepressant compared to other depression medications in their area of residence [9]. Strøm et al. revealed similar results [10]. Aslan et al. believed amitriptyline was prescribed more frequently, leading to a greater incidence of poisoning associated with it [9].
In our study, 29.6% of patients had a history of abuse. Another study showed similar results [6]. Overall, these results indicate that individuals with a history of abuse or previous suicide attempts are at a higher risk of repeating these behaviors. This issue highlights the importance of carefully examining these patients’ medical and psychological history.
We found that the majority of patients were related to suicide attempts (86.3%), which aligns with other studies [6]. This consistency suggests that the use of TCAs continues to be a prevalent method of suicide among people who use these medications. This situation underscores the necessity of being vigilant regarding the mental health of patients prescribed these drugs and emphasizes the importance of closely monitoring their access to them.
According to the results, 73% of the patients were hospitalized in the poisoning department, indicating that this patient group experienced mild poisoning severity. In a study by Gheshlaghi et al., 62% of patients with TCA poisoning were also reported to have mild severity [5], which aligns closely with our results. Conversely, Saleh et al. found that 92% of patients exhibited mild poisoning severity [6]. However, Saleh et al.’s assessment of poisoning severity was based on the need for intubation, which differed from our study’s methodology. Additionally, our study revealed a significant relationship between the types of TCAs and the severity of poisoning. Notably, amitriptyline was associated with the highest frequency of hospitalization in the CCU.
Rhabdomyolysis was identified in 4.7% of the patients. The analysis of TCA types related to rhabdomyolysis showed a significant association, with amitriptyline being the most frequently implicated (9 cases). Babulovska et al. reported an 8.3% prevalence of rhabdomyolysis among those poisoned with antidepressants [11]. The higher prevalence in their study may stem from their broader evaluation criteria. Our study defined rhabdomyolysis based on a CPK level greater than 975 IU. In contrast, Babulovska et al. categorized rhabdomyolysis severity using a wider range: Mild (250–1500 IU), moderate (1500–10,000 IU), and severe (greater than 10,000 IU). This broader definition allowed them to identify milder cases that our fixed threshold may have missed.
Additionally, Caruana et al. examined rhabdomyolysis in TCA-poisoned patients and noted that amitriptyline abuse was associated with this condition. While their findings align with ours [12], they did not specify the prevalence of rhabdomyolysis in their cohort. Our results confirm that amitriptyline posed the highest risk for rhabdomyolysis among TCAs. This consistency with other studies highlights the need for heightened awareness of rhabdomyolysis symptoms in patients with amitriptyline poisoning to prevent serious complications. Although no correlation was observed between mortality and the age or gender of patients in the present study, a significant relationship emerged between rhabdomyolysis and death. Specifically, of the 233 patients with poisoning, 2 out of 4 fatalities (0.85%) occurred in individuals with rhabdomyolysis. In contrast, Mousavi et al. reported a mortality rate of 4.1% [13], while Faraji Dana et al. found a mortality rate of 8.8% associated with rhabdomyolysis [14]. These findings suggest that the mortality rate in our study is lower than in others, which may be attributed to several factors, including quicker and more effective therapeutic interventions, variations in the severity of rhabdomyolysis, and differences in patient demographics. Additionally, geographical variations and the resources available at treatment centers could also influence the results.
The results indicated that seizures were observed in 10.7% of the individuals. In the study by Saleh et al., seizures occurred in 8% of patients [6]. Also, Citak et al. evaluated patients with seizures due to poisoning concerning the causes, frequencies, and complications of seizures, and found that TCA poisoning was the leading cause of seizures [15].
Moreover, the present study had a significant relationship between the TCA types and seizures. In this regard, amitriptyline was the most frequently seizure-causing drug (48%). Similarly, in Citak et al.’s study, out of 26 patients, the highest frequency of seizures was related to amitriptyline (34%) [15]. These studies are consistent with the findings of the present study.
The assessment of agitation among patients revealed that agitation was present in 42.9% of the individuals. Saleh et al. showed agitation in 34% of patients [6]. In Aslan et al.’s study, agitation was observed in 37.5% of patients [9].
In our study, mydriasis was found in 39.05% of the patients and 52.3% of patients exhibited dry skin and mucous membranes. In the study by Gheshlaghi et al., 64.1% of patients experienced mydriasis [5]. Aslan et al. revealed the occurrence of dry skin and mucous membranes in patients with amitriptyline poisoning, with a prevalence rate of 12.5% [9].
Based on our findings, a decrease in blood pressure was observed in 18.5% of the patients. Saleh et al. also reported that blood pressure drop was caused by TCA compounds in 15% of patients [6], which is almost in line with the findings of our study. In the study by Aslan et al., only 5% of patients poisoned with amitriptyline experienced a decrease in blood pressure [9]. The differences in blood pressure drop among the studies might be due to the use of different doses of TCA [16].
According to our results, tachycardia was observed in 56.2% of patients. The findings of other studies are almost in line with our results [6, 9].
The shock was observed in 2.6% of the patients and QRS complex prolongation was observed in 14.16%. In the study conducted by Aslan et al., a QRS complex prolongation was observed in 15% of patients with amitriptyline poisoning [9], which was consistent with our findings. In contrast, Gheshlaghi et al, observed a wide QRS complex in 36.95% of patients [5], while Saleh et al. reported a wide QRS complex in 5% of patients. A tall R wave in the aVR lead was observed in 10.7% of the patients [6]. Gheshlaghi et al. indicated that the mean R wave size in aVR decreased during hospitalization [5]. Variations in ECG measurement techniques and the timing of ECG recordings post-poisoning may account for the differences observed across studies. Our study and other studies revealed a significant association between prolonged QRS duration and increased mortality [17]or the need for intubation [6, 18]. These results suggest that abnormal ECG changes, particularly QRS prolongation, are linked to more severe clinical conditions and the necessity for supportive measures, like intubation. Thus, ECG changes can serve as valuable indicators for predicting the severity of intoxication and guiding therapeutic interventions.
As indicated, an increase in WBC count was observed in 12.44% of patients, which was similar to other research [9]. The findings showed that increased and decreased potassium levels were observed in 5.15% and 5.57% of patients, respectively. Gheshlaghi et al. showed a decrease in potassium levels after 12 hours compared to admission time, followed by an increase that reached the initial level [5]. Mirrakhimov et al. reported that 9% of patients with TCA poisoning had a decrease in potassium levels [19]. Moreover, Ay et al. reported hypokalemia caused by amitriptyline poisoning in 12.5% of patients [18].
In our study, an increase and a decrease in HCO3 levels were observed in 3.8% and 8.2% of patients, respectively. Aslan et al. showed a decrease in HCO3 in 5% of patients [9]. Additionally, increases and decreases in PCO2 were found in 6.4% and 3% of patients, respectively.
Our study found increased and decreased pH values in 2.1% and 8.2% of patients, respectively. Gheshlaghi et al. observed a significantly increasing pattern of pH [5].
The results indicated that out of 231 patients, 102 patients (44.15%) took the drug simultaneously. Also, the highest frequency of simultaneous drug use was associated with amitriptyline. Saleh et al. reported that 16% of TCA-poisoned patients used drugs simultaneously [6].
The most frequent treatment for TCA poisoning in our patients was sodium bicarbonate (51%). The study by Suksaranjit et al. aligned with our findings, as they reported that their patients were treated with sodium bicarbonate [20]. The benefits of administering sodium bicarbonate in cases of TCA poisoning are due to its ability to increase the electrochemical gradient across cardiac cell membranes, potentially mitigating the sodium channel blockade caused by TCAs [20]. In addition, intubation was observed in 8.2% of TCA-poisoned patients. Saleh et al. reported that 7.8% of patients underwent tracheal tube intubation, which was in line with our study [6].
In the current study, 1.7% of patients died. The frequency of death in the study by Strøm et al. was 2% [10]. Caksen et al. studied amitriptyline intoxication in childhood, examining 44 children and observing a frequency of death of 4.54% due to amitriptyline [21]. Bronstein et al. studied the dosages of anti-depressant compounds and observed that the mortality rate was 4% [22]. The findings of these studies were almost in line with our results. Babulska et al. investigated 140 patients with different poisoning agents and reported that among these patients, 12 cases of poisoning with TCAs were noted, but no deaths occurred in these 12 patients [11]. These comparisons indicate a low rate of death in TCA poisoning, and the differences between studies may be attributed to variations in the severity of poisoning, the type of compound consumed, and patient-related factors.
Conclusion
In conclusion, TCA poisoning remains a significant challenge in managing poisoned patients, particularly across different regions. The findings indicated that nortriptyline and amitriptyline have the highest rates of poisoning, likely due to their prevalent prescription in Iran. The higher incidence of poisoning among women, coupled with suicide as a primary motive, underscores the need for attention to psychological issues and careful monitoring of these medications. Cardiac complications, such as tachycardia and QRS complex prolongation on the ECG, are critical indicators of poisoning. Prompt treatment with sodium bicarbonate, along with the management of severe conditions, like seizures and hypotension, can be lifesaving. Ultimately, the results of this research emphasize the importance of accurately predicting the severity of poisoning and implementing swift, effective treatment strategies to enhance patient care and reduce complications and mortality.
It is recommended that further research be conducted to compare the toxicity of TCAs with newer-generation antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). These studies should assess the severity of toxicity, side effects, and mortality rates related to TCAs compared to SSRIs and SNRIs. Such studies should evaluate clinical symptoms, cardiac and neurological complications, and the necessity for immediate therapeutic interventions among these drug groups to determine which is safer.
Ethical Considerations
Compliance with ethical guidelines
This retrospective cross-sectional study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran, (Code: IR.SSU.MEDICINE.REC.1402.257). Patients gave written informed consent, and strict confidentiality was upheld regarding all patient information.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Supervision and data gathering: Hamid Owliaey; Data analysis: Komeil Aghazadeh-Habashi and Sareh Rafatmagham; Writing the original draft: Negar Zahir Mirdamadi, Hamid Reza Jamshidi, and Khashayar Moravej; Review and editing: Farhad Farnaghi, Hamid Reza Ghasemirad, and Raheleh Kadiouri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate all the authors of the included studies.
References
Depression is a debilitating, financially burdensome, and lethal disorder [1-4]. Currently, the treatment of depression is carried out by specialists through a combination of psychotherapy, pharmacological therapy, electroshock, and lifestyle modifications, and the beneficial effects of these strategies are mainly synergistic [2-4]. Pharmacological treatment is a key component in the treatment of depression, particularly in severe cases and circumstances that necessitate rapid intervention [2]. Tricyclic antidepressants (TCAs) are a class of pharmacological medications that are used in the treatment of major depressive disorder (MDD), nocturnal enuresis, and chronic pain [5, 6]. TCAs initially launched in the market in 1959 [7]. These medications exert their effect by blocking the reabsorption of neurotransmitters, like serotonin and norepinephrine, which can influence mood, focus, and pain perception in individuals [8].
TCA intoxication can happen in instances of suicide and accidental overdose. The consumption of TCAs could cause neurological complications, such as confusion, seizures, as well as cardiac issues, including tachycardia, QTc prolongation, widened QRS complex, and hypotension. Other adverse effects of TCAs include blurred vision, constipation, xerostomia, confusion, and urinary retention [8].
Considering the multiple complications related to TCA poisoning, as well as the availability of these drugs and their potential for abuse, this retrospective cross-sectional study aimed to investigate patients with TCA poisoning who were admitted to Shah Vali Hospital in Yazd, Iran, and Shahid Beheshti Taft Hospital in Taft, Yazd, Iran, between 2014 and 2023. The study also sought to evaluate the frequency of clinical, paraclinical, and prognostic findings in these patients.
Materials and Methods
Inclusion and exclusion criteria
This retrospective cross-sectional study included all poisoned patients with TCAs who were admitted to Shah Vali Hospital, Yazd, Iran, and Shahid Beheshti Hospital, Taft, Yazd, Iran, from 2013 to 2022. The medical history and clinical examination of the patients were consistent with the symptoms of TCA poisoning. Moreover, this study excluded patients poisoned with other agents or unknown agents, and patients with incomplete medical records.
Data collection
The medical records and the hospital information system (HIS) were reviewed to collect the demographic characteristics and clinical findings of poisoned patients with TCAs. The clinical findings included neurological findings, cardiovascular findings, paraclinical findings, therapeutic interventions, outcomes, and mortality of poisoned patients with TCAs.
The demographic characteristics included age, gender, marital status, education, hospitalization time, the cause of taking drugs, the history of abuse, the severity of the disease—in terms of hospitalization in the intensive care unit (ICU) or poisoning department—and rhabdomyolysis (CPK >975 IU/L).
The neurological findings included agitation, seizures, and pupillary mydriasis. Cardiovascular findings included fluctuating changes in blood pressure (BP), tachycardia, the morphology of the R wave in lead aVR, and QRS complex prolongation. Paraclinical findings included the levels of white blood cells (WBC), potassium (K), arterial blood gas/ venous blood gas (ABG/VBG), and blood pH. Therapeutic interventions included the administration of dopamine, sodium bicarbonate, norepinephrine, and intubation with a tracheal tube.
Statistical analysis
SPSS software, version 23 (SPSS Inc., Chicago, IL, USA) was utilized for statistical analysis. Qualitative variables were presented as frequencies (percentages). The statistical differences between groups were investigated by the chi-square and Fisher’s exact tests. All statistical analyses were conducted using a two-tailed approach. P<0.05 was considered statistically significant.
Results
This retrospective cross-sectional study included 233 poisoned patients with TCAs. Table 1 summarizes the demographic characteristics.
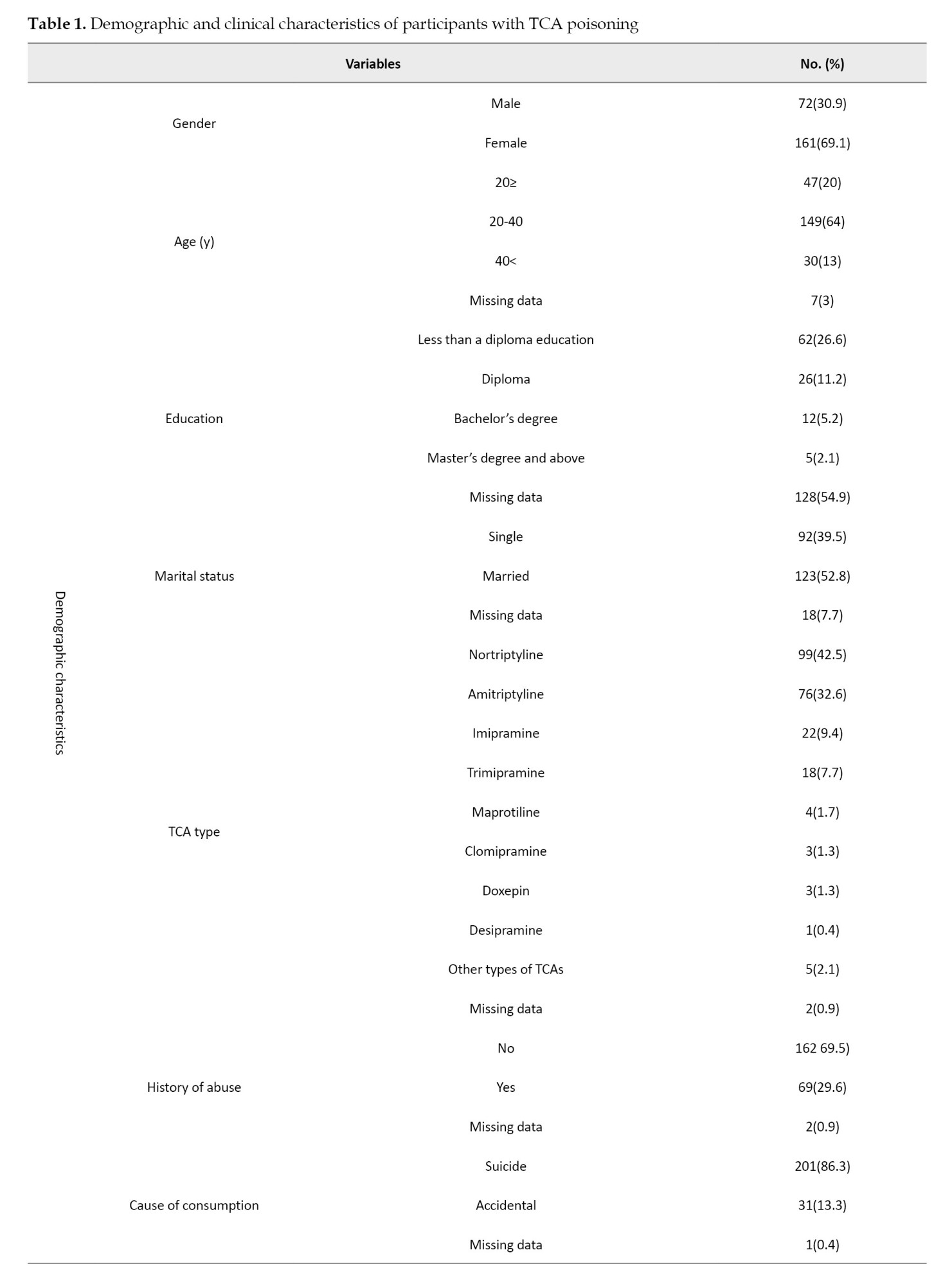
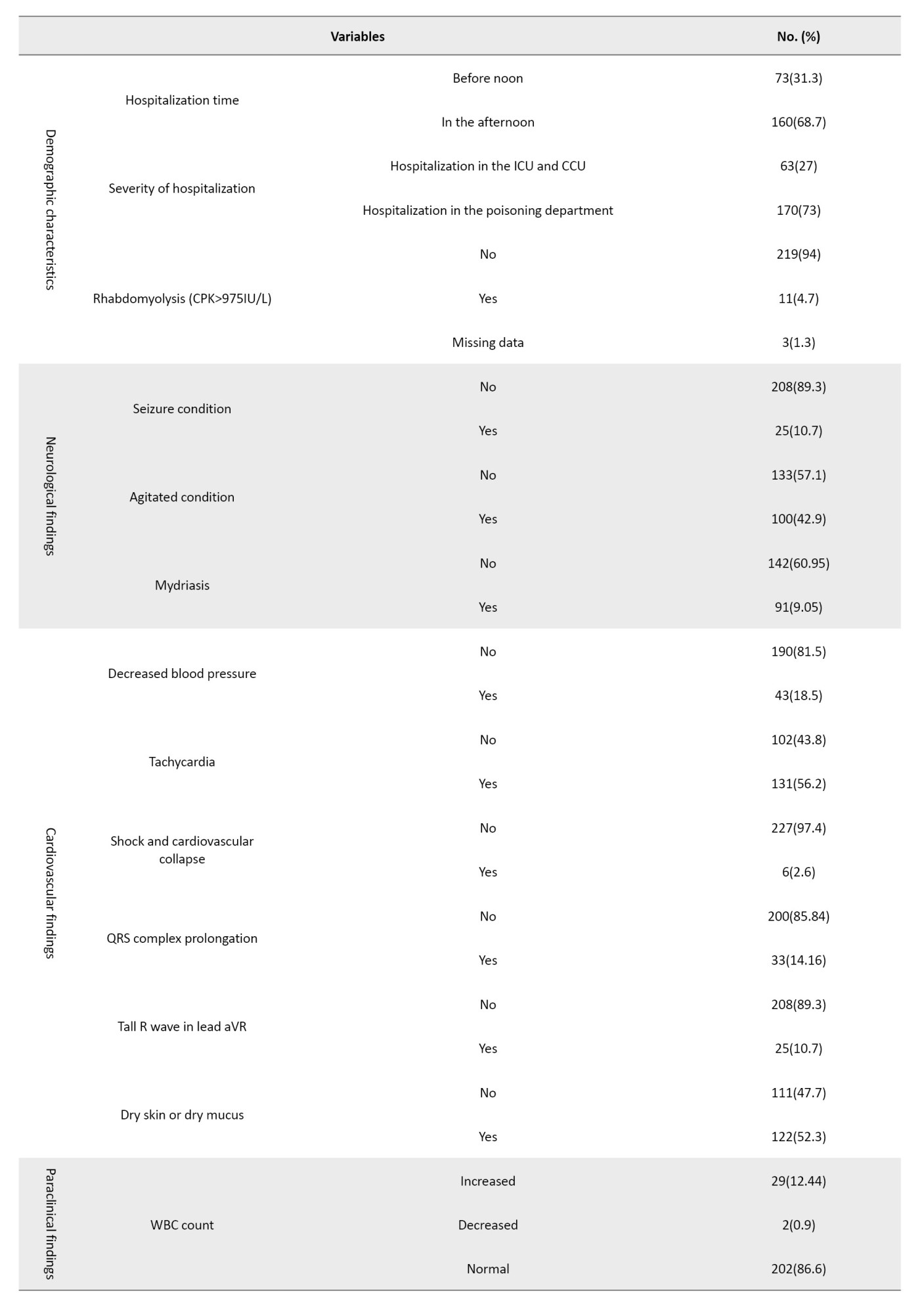
The most TCA-poisoned patients were female (69.1%). The age range of these patients was 2 to 67 years with a mean age of 28.11 years and the patients aged 20-40 years were more significantly impacted by TCA poisoning (64%). Analysis of the patient’s education and marital status showed that the highest frequency of TCA-poisoned patients was related to individuals with less than a diploma education (6.26%) and married individuals, comprising 52.8% of the cases. The most commonly reported TCAs were nortriptyline (42.5%) and amitriptyline (32.6%). Determining the frequency of previous abuse history among patients revealed that a history of previous abuse was seen in 29.6% of patients. The data indicated that the majority of patients had a history of suicide attempts (86.3%). Also, 68% of the patients were hospitalized during the afternoon. According to the results, 73% of the patients were hospitalized in the poisoning department. Rhabdomyolysis was identified in 4.7% of the patients. Seizures were observed in 10.7% of the individuals. The assessment of agitation frequency among patients revealed that agitation was present in 42.9% of the individuals. Mydriasis was observed in 39.05% of the patients.
A decrease in blood pressure was observed in 18.5% of the patients. Tachycardia was seen in 56.2% of cases. The shock was observed in 2.6% of the patients. QRS complex prolongation was observed in 14.16% of the patients. The results presented in Table 1 indicated that a tall R wave in the augmented vector right (aVR) lead was observed in 10.7% of the patients. Additionally, 52.3% of patients exhibited dry skin and mucous membranes. An increase and decrease in WBC count was observed in 12.44% and 0.9% of patients, respectively. The findings showed that increased and decreased potassium levels were observed in 5.15% and 5.57% of patients, respectively. Increases and decreases in HCO3 levels were observed in 3.8% and 8.2% of patients, respectively. Moreover, increases and decreases in PCO2 were found in 6.4% and 3%, respectively. As indicated, increased and decreased pH levels were observed in 2.1% and 8.2% of patients, respectively. The administration of dopamine, bicarbonate, and norepinephrine was noted in 2.6%, 51.1%, and 2.6% of the patients, respectively. Examining the frequency of patient mortality showed that 1.7% of patients died.
Table 2 presents a comparative analysis of the association between various demographic and other variables and the nine categories of TCAs.
There was a notable relationship between TCA type and gender (P=0.004). Among the 160 women studied, 81(50.62%) were prescribed nortriptyline, whereas among the 71 men, 36(50.70%) were prescribed amitriptyline.
There was no significant difference between the TCA types and age (P=0.122). There was a significant relationship between TCA type and the severity of the disease (P=0.001). Specifically, among the 63 cases hospitalized in the ICU and CCU, amitriptyline was the most frequently prescribed, accounting for 26 cases (41.2%).
There was a significant relationship between the frequency of TCA types and the occurrence of rhabdomyolysis (P=0.033). Notably, among the 11 cases of rhabdomyolysis identified, 9 cases (81.81%) were associated with amitriptyline.
There was a significant relationship between the frequency of TCA types and the occurrence of seizures (P=0.002). Specifically, among the 25 individuals experiencing seizures, the highest frequency was associated with amitriptyline, accounting for 12 cases (48%).
There was a significant relationship between the TCA types and the method of drug administration (P=0.004). This suggests a noteworthy relationship between the type of TCA used and the manner of its administration. Notably, amitriptyline exhibited the highest frequency of concurrent drug use, accounting for 43 out of 102 cases (42.2%).
Table 3 presents a comparative analysis of the association between mortality and other variables.
There was no association between the frequency of mortality and gender and age (P=0.797 and P=0.527, respectively). There was a significant association between the frequency of death and rhabdomyolysis (P=0.001). This suggests a meaningful relationship between mortality and the presence of rhabdomyolysis, with 2 out of 4 cases of death (50%) occurring in individuals with this condition. Additionally, the findings reveal a significant association between mortality and QRS complex prolongation (P=0.038). This indicates a significant relationship between mortality and QRS complex lengthening, with 2 out of 4 cases of death (50%) involving patients who exhibited QRS complex prolongation.
Table 4 presents a comparative analysis of the association between QRS complex prolongation and other variables.
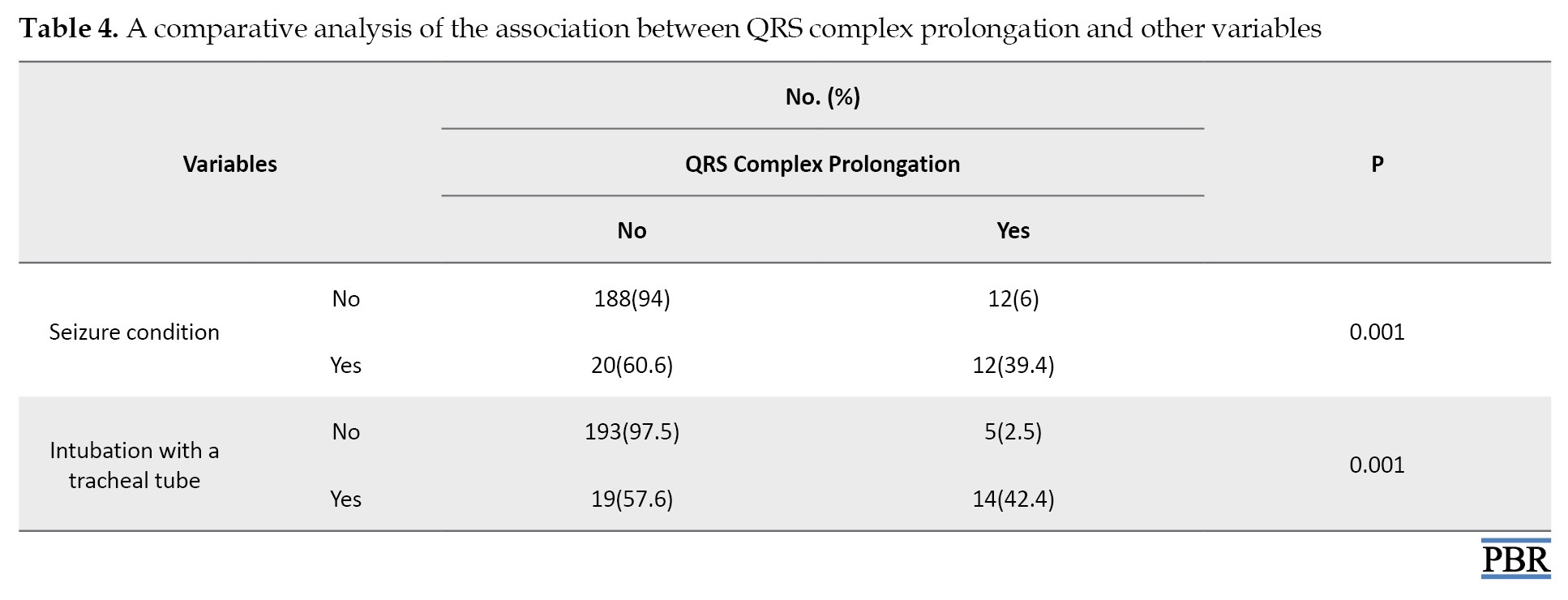
The findings in the table above revealed a significant association between the frequency of QRS complex lengthening and seizures (P=0.001). This suggests a noteworthy relationship between QRS complex prolongation and the occurrence of seizures, with 12 out of 32 cases of QRS complex prolongation (37.5%) involving patients who experienced seizures. Furthermore, the results indicated a significant association between the lengthening of the QRS complex and intubation with a tracheal tube (P=0.001). This finding highlights a significant relationship between QRS complex prolongation and tracheal intubation, as intubation was observed in 14 out of 33 cases of QRS complex prolongation (42.42%).
Discussion
This retrospective cross-sectional study investigated 233 TCA-poisoned patients with an age range of 2 to 67 years and with a mean age of 28.11 years between 2013 and 2022. Gheshlaghi et al. found 92 cases of TCA-poisoned patients with a mean age of 27.5 and an age range of 16–65 over two years [5]. In our study, similar to Saleh et al., the majority of patients were in the age group of 20-40 years [6]. These similarities indicate that TCA poisoning occurs more frequently in young and middle-aged groups. These findings suggest that young and middle-aged individuals, who may be at higher risk for various reasons such as depression or easy access to these drugs, constitute the majority of poisoning cases.
According to our findings, most of the TCA-poisoned patients were female (69.1%). Similarly, females predominated in other studies [5, 6]. The results of this study indicate that TCA toxicity was more common in women than in men.
Based on the patients’ education and marital status, people with less than a diploma education (26.6%) and married individuals (52.8%) comprised the highest frequency of TCA-poisoned patients. Based on Aslan et al.’s study, 47.5% of TCA-poisoned individuals were married, and 37% had less than a diploma education, respectively [9].
The majority of patients were poisoned with nortriptyline (42.5%) and amitriptyline (32.6%). Other studies align with our study [5, 6, 9]. Aslan et al. reported that the higher prevalence of amitriptyline poisoning can be attributed to the lower cost of this antidepressant compared to other depression medications in their area of residence [9]. Strøm et al. revealed similar results [10]. Aslan et al. believed amitriptyline was prescribed more frequently, leading to a greater incidence of poisoning associated with it [9].
In our study, 29.6% of patients had a history of abuse. Another study showed similar results [6]. Overall, these results indicate that individuals with a history of abuse or previous suicide attempts are at a higher risk of repeating these behaviors. This issue highlights the importance of carefully examining these patients’ medical and psychological history.
We found that the majority of patients were related to suicide attempts (86.3%), which aligns with other studies [6]. This consistency suggests that the use of TCAs continues to be a prevalent method of suicide among people who use these medications. This situation underscores the necessity of being vigilant regarding the mental health of patients prescribed these drugs and emphasizes the importance of closely monitoring their access to them.
According to the results, 73% of the patients were hospitalized in the poisoning department, indicating that this patient group experienced mild poisoning severity. In a study by Gheshlaghi et al., 62% of patients with TCA poisoning were also reported to have mild severity [5], which aligns closely with our results. Conversely, Saleh et al. found that 92% of patients exhibited mild poisoning severity [6]. However, Saleh et al.’s assessment of poisoning severity was based on the need for intubation, which differed from our study’s methodology. Additionally, our study revealed a significant relationship between the types of TCAs and the severity of poisoning. Notably, amitriptyline was associated with the highest frequency of hospitalization in the CCU.
Rhabdomyolysis was identified in 4.7% of the patients. The analysis of TCA types related to rhabdomyolysis showed a significant association, with amitriptyline being the most frequently implicated (9 cases). Babulovska et al. reported an 8.3% prevalence of rhabdomyolysis among those poisoned with antidepressants [11]. The higher prevalence in their study may stem from their broader evaluation criteria. Our study defined rhabdomyolysis based on a CPK level greater than 975 IU. In contrast, Babulovska et al. categorized rhabdomyolysis severity using a wider range: Mild (250–1500 IU), moderate (1500–10,000 IU), and severe (greater than 10,000 IU). This broader definition allowed them to identify milder cases that our fixed threshold may have missed.
Additionally, Caruana et al. examined rhabdomyolysis in TCA-poisoned patients and noted that amitriptyline abuse was associated with this condition. While their findings align with ours [12], they did not specify the prevalence of rhabdomyolysis in their cohort. Our results confirm that amitriptyline posed the highest risk for rhabdomyolysis among TCAs. This consistency with other studies highlights the need for heightened awareness of rhabdomyolysis symptoms in patients with amitriptyline poisoning to prevent serious complications. Although no correlation was observed between mortality and the age or gender of patients in the present study, a significant relationship emerged between rhabdomyolysis and death. Specifically, of the 233 patients with poisoning, 2 out of 4 fatalities (0.85%) occurred in individuals with rhabdomyolysis. In contrast, Mousavi et al. reported a mortality rate of 4.1% [13], while Faraji Dana et al. found a mortality rate of 8.8% associated with rhabdomyolysis [14]. These findings suggest that the mortality rate in our study is lower than in others, which may be attributed to several factors, including quicker and more effective therapeutic interventions, variations in the severity of rhabdomyolysis, and differences in patient demographics. Additionally, geographical variations and the resources available at treatment centers could also influence the results.
The results indicated that seizures were observed in 10.7% of the individuals. In the study by Saleh et al., seizures occurred in 8% of patients [6]. Also, Citak et al. evaluated patients with seizures due to poisoning concerning the causes, frequencies, and complications of seizures, and found that TCA poisoning was the leading cause of seizures [15].
Moreover, the present study had a significant relationship between the TCA types and seizures. In this regard, amitriptyline was the most frequently seizure-causing drug (48%). Similarly, in Citak et al.’s study, out of 26 patients, the highest frequency of seizures was related to amitriptyline (34%) [15]. These studies are consistent with the findings of the present study.
The assessment of agitation among patients revealed that agitation was present in 42.9% of the individuals. Saleh et al. showed agitation in 34% of patients [6]. In Aslan et al.’s study, agitation was observed in 37.5% of patients [9].
In our study, mydriasis was found in 39.05% of the patients and 52.3% of patients exhibited dry skin and mucous membranes. In the study by Gheshlaghi et al., 64.1% of patients experienced mydriasis [5]. Aslan et al. revealed the occurrence of dry skin and mucous membranes in patients with amitriptyline poisoning, with a prevalence rate of 12.5% [9].
Based on our findings, a decrease in blood pressure was observed in 18.5% of the patients. Saleh et al. also reported that blood pressure drop was caused by TCA compounds in 15% of patients [6], which is almost in line with the findings of our study. In the study by Aslan et al., only 5% of patients poisoned with amitriptyline experienced a decrease in blood pressure [9]. The differences in blood pressure drop among the studies might be due to the use of different doses of TCA [16].
According to our results, tachycardia was observed in 56.2% of patients. The findings of other studies are almost in line with our results [6, 9].
The shock was observed in 2.6% of the patients and QRS complex prolongation was observed in 14.16%. In the study conducted by Aslan et al., a QRS complex prolongation was observed in 15% of patients with amitriptyline poisoning [9], which was consistent with our findings. In contrast, Gheshlaghi et al, observed a wide QRS complex in 36.95% of patients [5], while Saleh et al. reported a wide QRS complex in 5% of patients. A tall R wave in the aVR lead was observed in 10.7% of the patients [6]. Gheshlaghi et al. indicated that the mean R wave size in aVR decreased during hospitalization [5]. Variations in ECG measurement techniques and the timing of ECG recordings post-poisoning may account for the differences observed across studies. Our study and other studies revealed a significant association between prolonged QRS duration and increased mortality [17]or the need for intubation [6, 18]. These results suggest that abnormal ECG changes, particularly QRS prolongation, are linked to more severe clinical conditions and the necessity for supportive measures, like intubation. Thus, ECG changes can serve as valuable indicators for predicting the severity of intoxication and guiding therapeutic interventions.
As indicated, an increase in WBC count was observed in 12.44% of patients, which was similar to other research [9]. The findings showed that increased and decreased potassium levels were observed in 5.15% and 5.57% of patients, respectively. Gheshlaghi et al. showed a decrease in potassium levels after 12 hours compared to admission time, followed by an increase that reached the initial level [5]. Mirrakhimov et al. reported that 9% of patients with TCA poisoning had a decrease in potassium levels [19]. Moreover, Ay et al. reported hypokalemia caused by amitriptyline poisoning in 12.5% of patients [18].
In our study, an increase and a decrease in HCO3 levels were observed in 3.8% and 8.2% of patients, respectively. Aslan et al. showed a decrease in HCO3 in 5% of patients [9]. Additionally, increases and decreases in PCO2 were found in 6.4% and 3% of patients, respectively.
Our study found increased and decreased pH values in 2.1% and 8.2% of patients, respectively. Gheshlaghi et al. observed a significantly increasing pattern of pH [5].
The results indicated that out of 231 patients, 102 patients (44.15%) took the drug simultaneously. Also, the highest frequency of simultaneous drug use was associated with amitriptyline. Saleh et al. reported that 16% of TCA-poisoned patients used drugs simultaneously [6].
The most frequent treatment for TCA poisoning in our patients was sodium bicarbonate (51%). The study by Suksaranjit et al. aligned with our findings, as they reported that their patients were treated with sodium bicarbonate [20]. The benefits of administering sodium bicarbonate in cases of TCA poisoning are due to its ability to increase the electrochemical gradient across cardiac cell membranes, potentially mitigating the sodium channel blockade caused by TCAs [20]. In addition, intubation was observed in 8.2% of TCA-poisoned patients. Saleh et al. reported that 7.8% of patients underwent tracheal tube intubation, which was in line with our study [6].
In the current study, 1.7% of patients died. The frequency of death in the study by Strøm et al. was 2% [10]. Caksen et al. studied amitriptyline intoxication in childhood, examining 44 children and observing a frequency of death of 4.54% due to amitriptyline [21]. Bronstein et al. studied the dosages of anti-depressant compounds and observed that the mortality rate was 4% [22]. The findings of these studies were almost in line with our results. Babulska et al. investigated 140 patients with different poisoning agents and reported that among these patients, 12 cases of poisoning with TCAs were noted, but no deaths occurred in these 12 patients [11]. These comparisons indicate a low rate of death in TCA poisoning, and the differences between studies may be attributed to variations in the severity of poisoning, the type of compound consumed, and patient-related factors.
Conclusion
In conclusion, TCA poisoning remains a significant challenge in managing poisoned patients, particularly across different regions. The findings indicated that nortriptyline and amitriptyline have the highest rates of poisoning, likely due to their prevalent prescription in Iran. The higher incidence of poisoning among women, coupled with suicide as a primary motive, underscores the need for attention to psychological issues and careful monitoring of these medications. Cardiac complications, such as tachycardia and QRS complex prolongation on the ECG, are critical indicators of poisoning. Prompt treatment with sodium bicarbonate, along with the management of severe conditions, like seizures and hypotension, can be lifesaving. Ultimately, the results of this research emphasize the importance of accurately predicting the severity of poisoning and implementing swift, effective treatment strategies to enhance patient care and reduce complications and mortality.
It is recommended that further research be conducted to compare the toxicity of TCAs with newer-generation antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). These studies should assess the severity of toxicity, side effects, and mortality rates related to TCAs compared to SSRIs and SNRIs. Such studies should evaluate clinical symptoms, cardiac and neurological complications, and the necessity for immediate therapeutic interventions among these drug groups to determine which is safer.
Ethical Considerations
Compliance with ethical guidelines
This retrospective cross-sectional study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran, (Code: IR.SSU.MEDICINE.REC.1402.257). Patients gave written informed consent, and strict confidentiality was upheld regarding all patient information.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Supervision and data gathering: Hamid Owliaey; Data analysis: Komeil Aghazadeh-Habashi and Sareh Rafatmagham; Writing the original draft: Negar Zahir Mirdamadi, Hamid Reza Jamshidi, and Khashayar Moravej; Review and editing: Farhad Farnaghi, Hamid Reza Ghasemirad, and Raheleh Kadiouri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate all the authors of the included studies.
References
- Kambou G. Ethnopharmacological survey of plants used in traditional medicine in Burkina Faso. J Ethnopharmacol. 2015; 174: 527-35. [DOI:10.1111/jcpp.12844] [PMID]
- Marwaha S, Palmer E, Suppes T, Cons E, Young AH, Upthegrove R. Novel and emerging treatments for major depression. Lancet. 2023; 401(10371):141-53. [DOI:10.1016/S0140-6736(22)02080-3] [PMID]
- Daly M, Sutin AR, Robinson E. Depression reported by US adults in 2017-2018 and March and April 2020. J Affect Disord. 2021; 278:131-5. [DOI:10.1016/j.jad.2020.09.065] [PMID]
- Fried EI, Flake JK, Robinaugh DJ. Revisiting the theoretical and methodological foundations of depression measurement. Nat Rev Psychol. 2022; 1(6):358-68. [DOI:10.1038/s44159-022-00050-2] [PMID]
- Gheshlaghi F, Eizadi-Mood N, Emamikhah-Abarghooeii S, Arzani-Shamsabadi M. Evaluation of serum sodium changes in tricyclic antidepressants toxicity and its correlation with electrocardiography, serum pH, and toxicity severity. Adv Biomed Res. 2012; 1:68. [DOI:10.4103/2277-9175.102972] [PMID]
- Saleh A, El-Galad G, El-Masry M, Abd El-Rhman A, Abd El-Salam M. Morbidity and mortality predictors in patients with acute tricyclic antidepressant toxicity. Ain Shams J Forensic Med Clin Toxicol. 2013; 20(1):1-9. [DOI:10.21608/ajfm.2013.19381]
- Dopheide JA. Recognizing and treating depression in children and adolescents. Am J Health Syst Pharm. 2006; 63(3):233-43. [DOI:10.2146/ajhp050264] [PMID]
- Moraczewski J, Awosika AO, Aedma KK. Tricyclic antidepressants. Treasure Island: StatPearls Publishing; 2023. [Link]
- Aslan Ş, Emet M, Cakir Z, Aköz A, Gür STA. Suicide attempts with amitriptyline in adults: A prospective, demographic, clinical study. Turk J Med Sci. 2011; 41(2):243-9. [DOI:10.3906/sag-0908-227]
- Strøm J, Sloth Madsen P, Nygaard Nielsen N, Bredgaard Sørensen M. Acute self-poisoning with tricyclic antidepressants in 295 consecutive patients treated in an ICU. Acta Anaesthesiol Scand. 1984; 28(6):666-70. [DOI:10.1111/j.1399-6576.1984.tb02142.x] [PMID]
- Babulovska A, Caparovska D, Velikj Stefanovska V, Simonovska N, Pereska Z, Petkovska L, et al. Comparison of rhabdomyolysis in acutely intoxicated patients with psychotropic and chemical substances. Folia Med. 2023; 65(3):407-14. [DOI:10.3897/folmed.65.e81145] [PMID]
- Caruana RJ, Dilworth LR, Williford PM. Acute rhabdomyolysis associated with an overdose of lorazepam, perphenazine and amitriptyline. N C Med J. 1983; 44(1):18-9. [PMID]
- Mousavi SR, Taghaddosinejad F, Talaee H, Zare GA, Sadeghi M, Rajaee P, et al. [Clinical and laboratory evaluation of rhabdomyolysis in 165 patients with severe acute poisonings (Persian)]. J Birjand Univ Med Sci. 2010; 17(2):136-42. [Link]
- Faraji Dana H, Heidari Jafari E, Ghorbani M, Elsagh A. [Study of prevalence of rhabdomyolysis due to poisoning and its relation with clinical findings of patients who have been admitted in Rajaie Hospital since 1397 (Persian)]. Alborz-Health. 2021; 10(2):249-54. [Link]
- Citak A, Soysal DD, Uçsel R, Karaböcüoglu M, Uzel N. Seizures associated with poisoning in children: Tricyclic antidepressant intoxication. Pediatr Int. 2006; 48(6):582-5. [DOI:10.1111/j.1442-200X.2006.02276.x] [PMID]
- Karimi I, Yakhchalian N, Fathi M, Miraghaee S. Pharmacogenomic considerations for prescribing the antidepressant fluoxetine: A review in personalized medicine. Universal J Pharm Res. 2022; 7(3):74-80. [DOI:10.22270/ujpr.v7i3.779]
- Miri SM, Jalali S, Karimi P. 712 Prediction of left ventricular dysfunction in basis of ventricular depolarisation time and electrical axis in patients with left bundle branch block. Eur J Heart Failure Suppl. 2006; 5(S1):164. [DOI:10.1016/S1567-4215(06)80463-7]
- Ay B, Fak AS, Toprak A, Göğüş YF, Oktay A. QT dispersion increases during intubation in patients with coronary artery disease. J Electrocardiol. 2003; 36(2):99-104. [DOI:10.1054/jelc.2003.50017] [PMID]
- Mirrakhimov AE, Ayach T, Barbaryan A, Talari G, Chadha R, Gray A. The role of sodium bicarbonate in the management of some toxic ingestions. Int J Nephrol. 2017; 2017:7831358. [DOI:10.1155/2017/7831358] [PMID]
- Suksaranjit P, Ratanapo S, Srivali N, Ahmed S, Cheungpasitporn W, Chongnarungsin D, et al. Electrocardiographic changes in tricyclic antidepressant toxicity. Am J Emerg Med. 2013; 31(4):751-2. [DOI:10.1016/j.ajem.2012.12.038] [PMID]
- Caksen H, Akbayram S, Odabaş D, Ozbek H, Erol M, Akgün C, et al. Acute amitriptyline intoxication: An analysis of 44 children. Hum Exp Toxicol. 2006; 25(3):107-10. [DOI:10.1191/0960327106ht511oa] [PMID]
- Bronstein AC, Spyker DA, Cantilena LR Jr, Green J, Rumack BH, Heard SE. 2006 annual report of the American association of poison control centers' national poison data system (NPDS). Clin Toxicol. 2007; 45(8):815-917. [DOI:10.1080/15563650701754763] [PMID]
Type of Study: Original Research |
Subject:
Toxicology
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |