Volume 10, Issue 3 (2024)
Pharm Biomed Res 2024, 10(3): 247-256 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Baharvand P, Vaez Z. Demographic, Clinical, and Laboratory Characteristics of Patients With COVID-19 Admitted to a Hospital in Khorramabad, Western Iran. Pharm Biomed Res 2024; 10 (3) :247-256
URL: http://pbr.mazums.ac.ir/article-1-617-en.html
URL: http://pbr.mazums.ac.ir/article-1-617-en.html
1- Department of Social Medicine, School of Medicine, Lorestan University of Medical Sciences, Khorramabad, Iran.
Full-Text [PDF 758 kb]
(586 Downloads)
| Abstract (HTML) (1941 Views)
Full-Text: (471 Views)
Introduction
In December 2019, the new coronavirus (COVID-19) was detected in Wuhan, China and spread rapidly worldwide. It affected the health systems and created a global health crisis. Iran’s Ministry of Health and Medical Education officially announced that two people in Qom City were infected with COVID-19 on February 19, 2020. This number later increased dramatically, and the disease spread to other parts of Iran. Studies on the course of the disease show that control and preventive measures significantly reduce the prevalence of COVID-19 and its mortality. Many studies have been conducted to investigate the risk factors affecting the death or recovery of patients with COVID-19 in Iran and other countries to provide comprehensive information in the field of treatment and control [1-12]. Mehri et al., in a systematic meta-analysis study, reported a significant association between death from COVID-19 and age, male gender, diabetes, hypertension, cardiovascular disease, cerebrovascular disease, chronic kidney disease, headache, and dyspnea. Moreover, they found a significant association between increased white blood cell (WBC), decreased lymphocytes, increased blood urea nitrogen (BUN), increased creatinine (Cr), vitamin D deficiency, and death from COVID-19 [1]. Arman et al., in a study on patients with COVID-19 in Tehran, Iran, reported that cough, respiratory distress, and fever were the most common symptoms of COVID-19. In their research, cancer, chronic lung diseases, and chronic neurologic diseases were the strongest risk factors for death in COVID-19 patients [8]. In Jalili et al.’s national cohort study on 28981 hospitalized patients with COVID-19 from 1034 hospitals in Iran, heart disease, asthma, chronic obstructive pulmonary disease, chronic kidney disease, cancer, and chronic liver disease had an association with death in patients with COVID-19 [13]. In Zali et al.’s study on 16016 hospitalized patients with COVID-19 in Tehran City, Iran, the highest total death rate was observed in patients aged >65 years (25.32%) with diabetes and cardiovascular diseases (38.46%), and cancer (35.79%) [14]. Nouri-Vaskeh et al. investigated the characteristics of 111 patients who died of COVID-19 in Tabriz City, northwest of Iran. According to their studies, dyspnea, cough, and fever were the most common symptoms. Among comorbidities, diabetes, hypertension, and cardiovascular diseases were more common among the deceased patients [15]. Sheikhi et al. assessed the demographic and clinical characteristics of 169 hospitalized patients with COVID-19 in Iranshahr, southeast of Iran. In their study, a history of hypertension was reported in 24.3%, heart disease in 22.5%, and diabetes in 12.4% of patients. Shortness of breath with 71.6% and cough with 69.8% were the most common symptoms, while chest pain with 7.7% was the least common. Of 169 patients, 146(86.4%) recovered, and 34(13.6%) died [16]. Talebi et al. compared the clinical and epidemiological characteristics of deceased and recovered patients with COVID-19 in Sabzevar, northeast of Iran. Of 178 patients, 85.4% recovered, and 14% died. Shortness of breath (72.5%) was the most common symptom, followed by cough (61.8%) and fever (48.9%). Moreover, 43.8% of all patients and 71.9% of deceased patients had at least one underlying disease. Increased WBC count, decreased lymphocyte, and increased neutrophils were significantly higher in deceased cases [17]. Haghighi et al. investigated the demographic, clinical, laboratory characteristics, and imaging features of patients with COVID-19 admitted to the intensive care unit (ICU) of hospitals in Rasht City, Northern Iran. Diabetes mellitus, hypertension, and chronic heart disease were the most common underlying diseases. Shortness of breath, fever, and cough were the most common symptoms. Ground-glass opacity was the most common lung CT scan finding, and an increase in the level of lactate dehydrogenase (LDH), erythrocyte sedimentation rate (ESR), C-reactive protein rate, neutrophil percentage, and lymphopenia were the most common laboratory findings in the patients. The mortality rate was 90.58% [18]. Ghelmani et al. investigated the risk factors associated with mortality in 932 patients with COVID-19 admitted to a hospital in Yazd, central Iran. The mortality rate was 9.6% (n=82). The identified risk factors were higher age, shortness of breath, history of cancer, hospitalization in the ICU, increased WBC count, and sodium deficiency [19].
Exploring the epidemiological features of COVID-19 and assessing underlying comorbidities among affected patients could help public health officials, decision-makers, and clinicians take the initiative in reducing the burden of this infectious disease and consequently controlling the pandemic. Although several studies have been recently performed to report specific epidemiological and clinical characteristics of COVID-19 patients in Iran, we found no study on the characteristics of hospitalized patients in Khorramabad, western Iran. In this regard, this epidemiological study aims to investigate the demographic, clinical, and laboratory characteristics of patients with COVID-19 admitted to a hospital in Khorramabad city to find the factors associated with death from COVID-19.
Materials and Methods
This research is a descriptive-analytical study with a cross-sectional design. The data of all patients with COVID-19 hospitalized in an educational hospital (Shahadaye Ashayer) affiliated with Lorestan University of Medical Sciences in the mid-year of 2021 were examined (n=555). The inclusion criteria were a definite diagnosis of COVID-19 (RT-PCR positive) and hospitalization in special units for coronavirus cases. The exclusion included the definite diagnosis of other respiratory diseases, flu, and respiratory problems unrelated to COVID-19 and incomplete medical files.
A researcher-made checklist was used to extract patients’ information, including demographic information (age, sex, occupation, educational level, marital status, place of residence), history of smoking, clinical symptoms, history of underlying diseases, and laboratory findings. The data were collected from the patient’s medical files by referring to the hospital’s medical data archive system. Then, they were analyzed in SPSS software, version 19, using descriptive statistics, independent t-test, and chi-square test. The significance level was set at 0.05.
Results
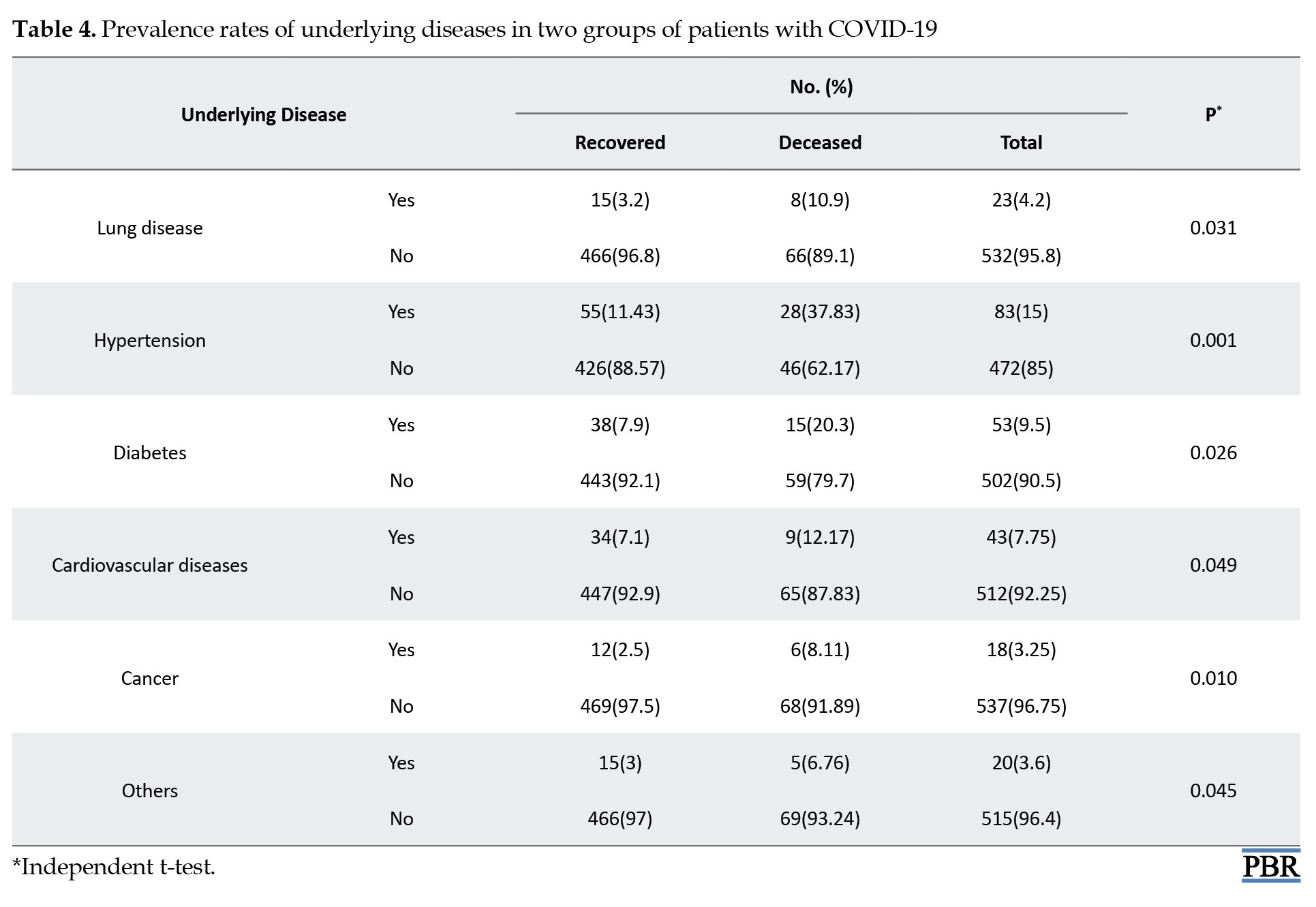
Among 555 patients, 295(53.1%) were male and 260(46.9%) were female. There were 481 recovered cases (86.7%) and 74 deceased cases (13.3%). The mean age of patients was 58.49±13.25 years, where recovered cases had a mean age of 55.08±10.91 years (range: 17-82 years), and the deceased cases had a mean age of 77.18±9.46 years (range: 56-87 years). According to the independent t-test results, the difference between the two groups regarding age was statistically significant (P<0.001). Most patients were married (n=419, 75.4%) with high school diplomas (n=223, 40.2%) and were living in urban areas (n=500, 90.2%) with no history of smoking (n=334, 60.2%). The personal characteristics of the patients in the deceased and recovered groups are presented in Table 1.
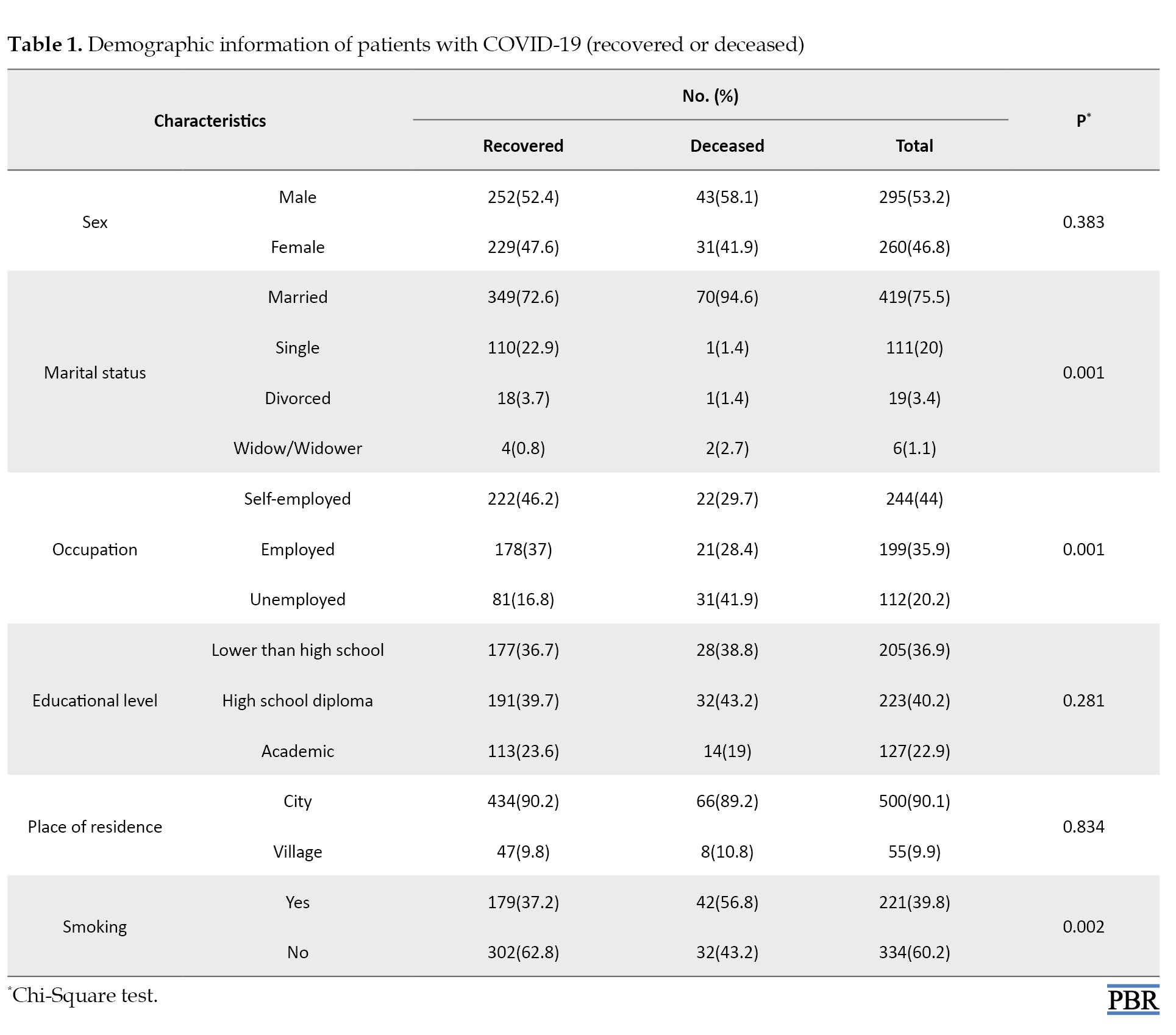
The results of the chi-square test showed that the differences between the two groups were statistically significant in terms of marital status (P=0.001), occupation (P=0.001), and history of smoking (P=0.002). No significant difference was found in terms of sex and place of residence (P>0.05) (Table 1).
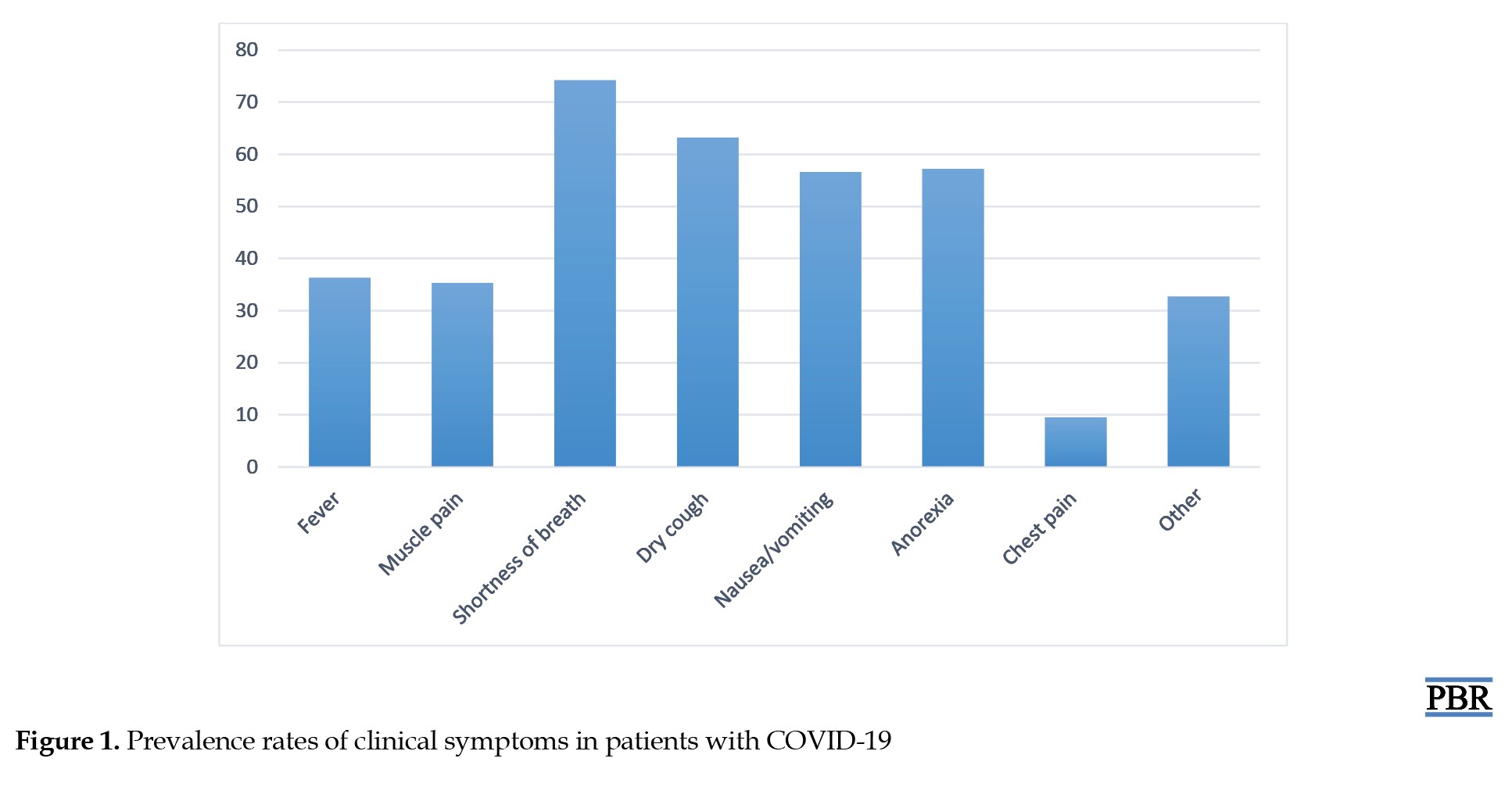
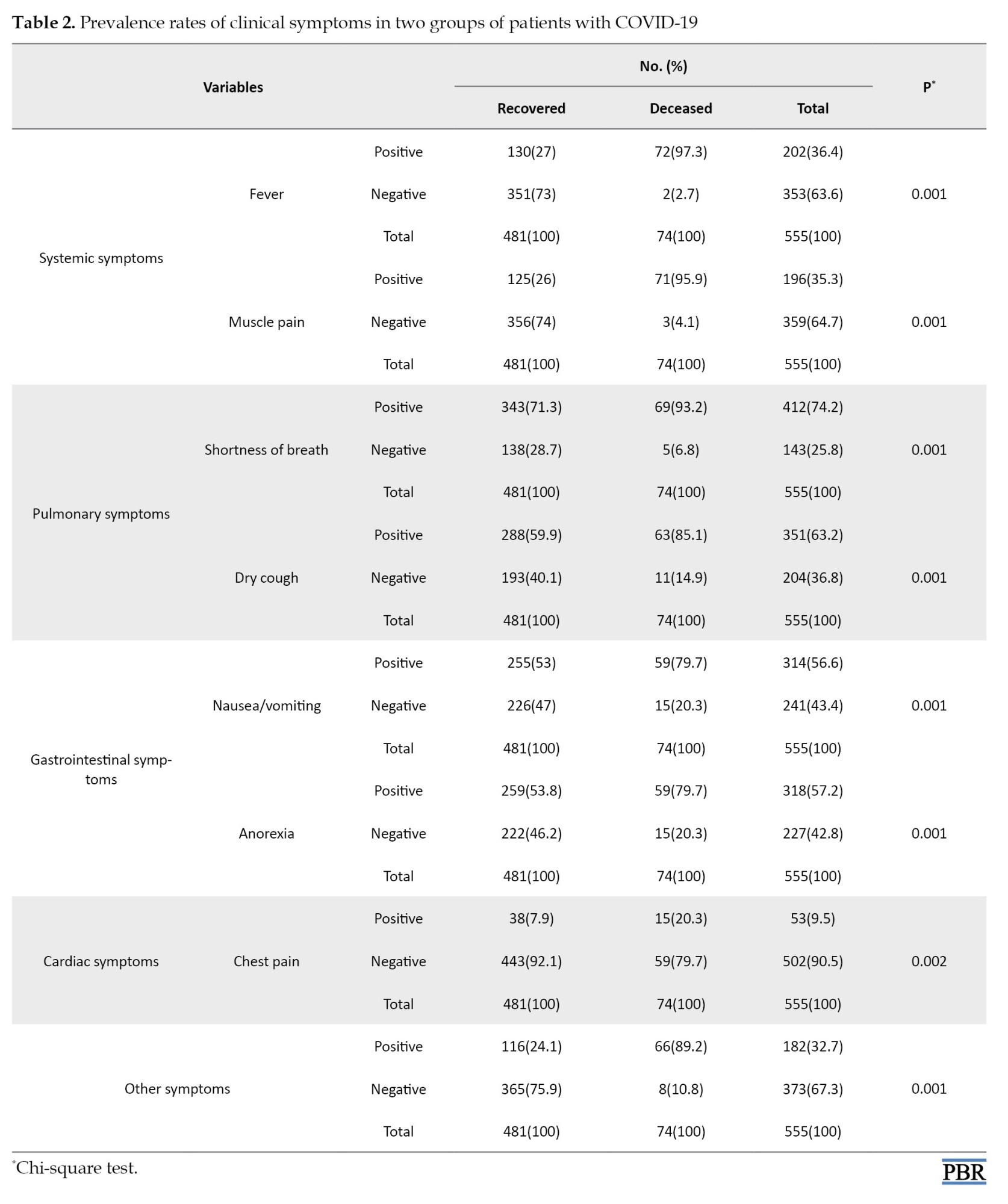
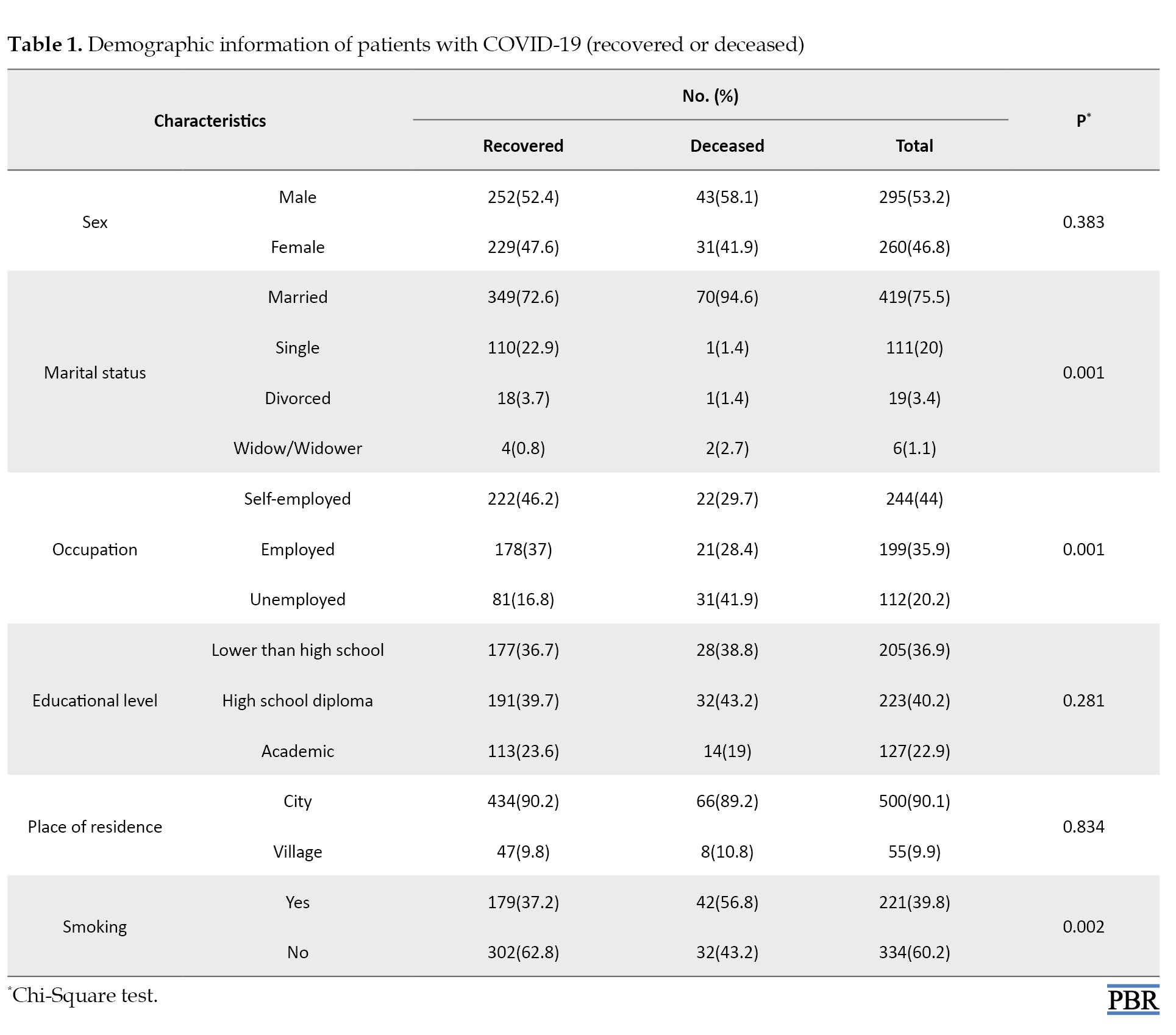
Regarding the clinical findings (Figure 1), the prevalence rates of fever and muscle pain (systemic symptoms) were 36.3% (n=202) and 35.3% (n=196), respectively. The prevalence of shortness of breath and dry cough (pulmonary symptoms) was 74.2% (n=412) and 63.2% (n=351), respectively. The prevalence of nausea/vomiting and anorexia (gastrointestinal symptoms) was 56.6% (n=314) and 57.2% (n=318), respectively. Chest pain had a low prevalence rate of 9.5% (n=53). The results of the chi-square test showed that the differences between the two groups were significant in terms of all clinical symptoms (P<0.05) (Table 2).
Regarding the laboratory findings, the means of WBC count, platelet count, and ESR in COVID-19 patients were 11.2±1.6 (×109/L), 250.13±98.18 (×109/L), and 82.25±2.3 (mm/h), respectively. The mean percentages of neutrophils, eosinophils, and lymphocytes (the components of WBCs) were 71.3±2.06%, 1.03±0.5%, and 25.03±1.07%. The mean levels of Cr, potassium (K), sodium (Na), and BUN were 2.01±0.01, 3.8±0.5, 137.7±1.08, and 32.7±4.08, respectively. Moreover, the mean levels of liver enzymes aspartate transaminase (AST), alkaline transaminase (ALT), and alkaline phosphatase (ALP) were 37.58±10.16, 36.43±9.24, and 181.04±93.99 (U/L), respectively. The laboratory findings of the patients for the deceased and recovered groups are presented in Table 3.
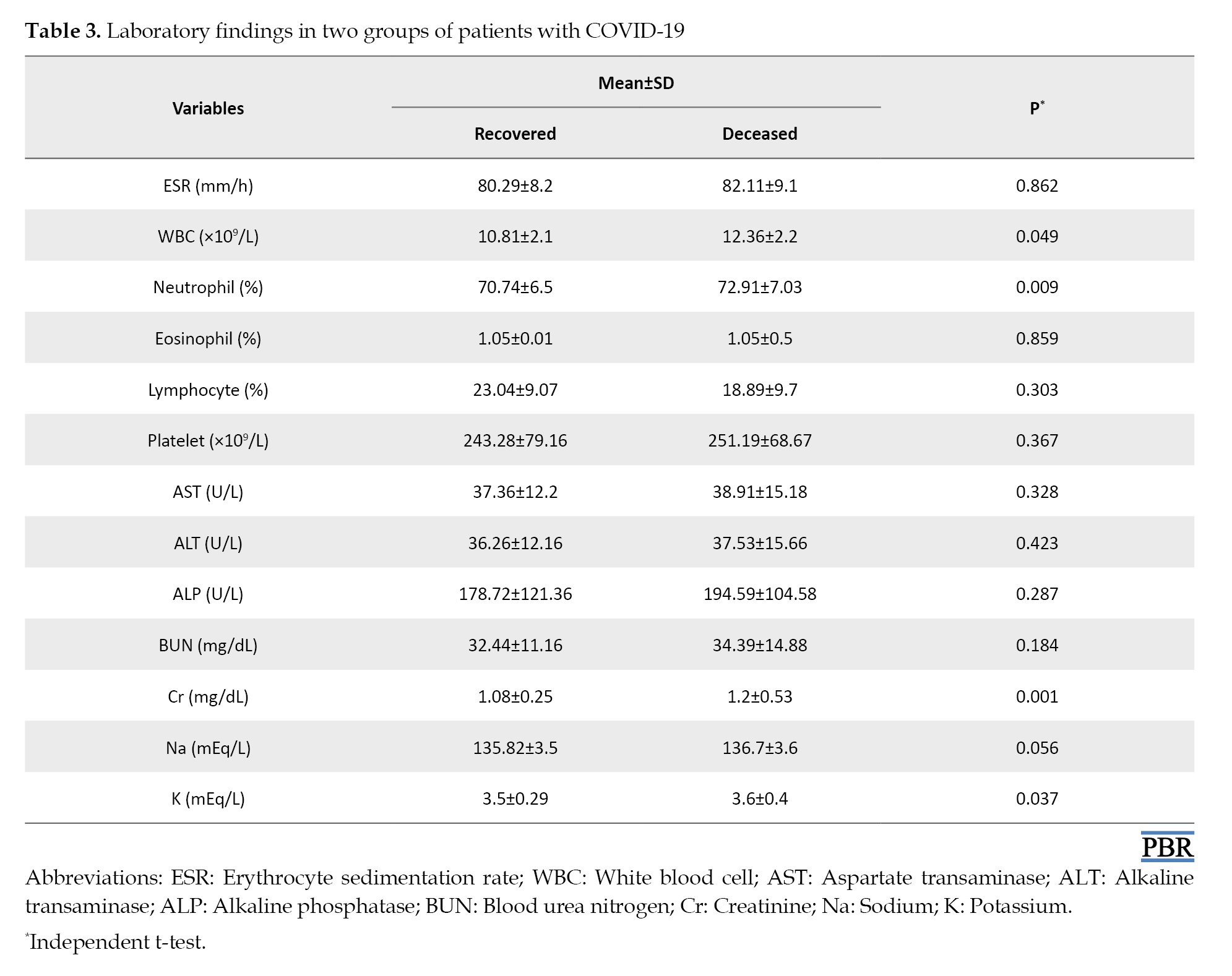
According to the results of the independent t-test, the difference between the recovered and deceased groups was statistically significant only in terms of WBC count (P=0.049; 10.81±2.1 vs 12.36±2.2), neutrophil percentage (P=0.009; 70.74±6.5% vs 72.91±7.03%), Cr level (P=0.001; 1.08±0.25 vs 1.2±0.53 mg/dL), and K level (P=0.037; 3.5±0.29 vs 3.6±0.4 mEq/L).
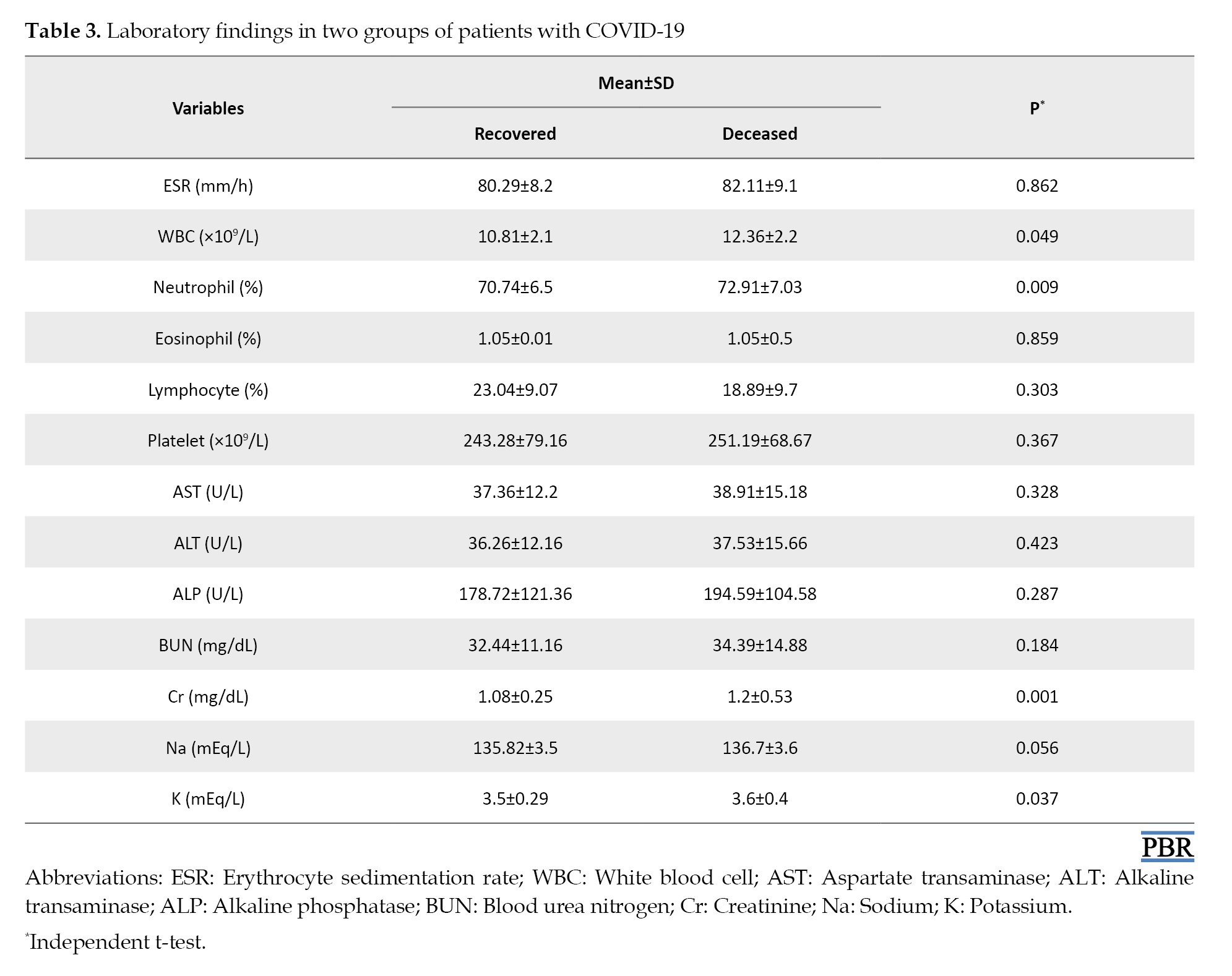
Regarding the underlying diseases, it was found that 103 out of 555 patients with COVID-19 had underlying diseases, 23(4.2%) had lung disease, 83(15%) hypertension, 53(9.5%) diabetes, 43(7.75%) cardiovascular diseases, 18(3.25%) cancer, and 20(3.6%) reported other diseases. Table 4 presents the frequency of underlying diseases for each group of deceased and recovered cases.
As can be seen, the frequency of underlying diseases was higher in the deceased cases than in the recovered patients, and this difference was significant in all underlying diseases (P<0.05).
Discussion
This study aimed to investigate the epidemiological and clinical characteristics of patients with COVID-19 admitted to a hospital in Khorramabad, Iran. The data of 555 patients were examined. The prevalence of mortality was reported 13.3% (n=74). This number is close to the prevalence rates reported by Sheikhi et al. (13.6%) in Iranshahr City and Talebi et al. (14%) in Sabzevar City [16-17] but lower than the death rate reported by Haghighi et al. (90.58%) on ICU patients in Rasht City [18], and higher than the rate reported by Ghelmani et al. (9.6%) in Yazd City [19]. In Grasselli et al.’s study in a city in Italy of 3988 hospitalized patients with COVID-19, the mortality rate was reported 915(53.4%) in the hospital [12]. This number is higher than the prevalence rate reported in our study. The difference in the mortality rates may be due to the difference in the disease severity in the studied patients and the quality of medical care provided by the studied hospitals.
In our study, the deceased patients had a mean age of 77.18±9.46 years (range: 56-87 years) and were older than the recovered cases with a mean age of 55.08±10.91 years. This difference was statistically significant. This finding is consistent with the results of previous studies in Iran [14, 16-19] and other countries [12], which reported that old age is a risk factor for death by COVID-19 in hospitalized patients. Another finding was that the death rate was significantly higher in hospitalized patients with a history of smoking tobacco (56.8%). Smoking can reduce the function of the immune system and is associated with a decrease in the number and proportion of circulating natural killer cells [ 20]. In a review study, Vardavas and Nikitara reported that smokers showed 1.4 times more severe symptoms of COVID-19 and approximately 2.4 times more likely to be admitted to ICU. They need more mechanical ventilation and die compared to non-smokers [21].
In this study, shortness of breath, dry cough, nausea/vomiting, and anorexia were the most prevalent clinical symptoms in patients with COVID-19, while chest pain had the lowest prevalence. All clinical symptoms were significantly related to the death of COVID-19. These results are consistent with the reports of Nouri-Vaskeh et al., Sheikhi et al., Talebi et al., Haghighi et al., and Gozidehkar et al. for hospitalized COVID-19 patients in other parts of Iran [15-18, 22]. In our study, the most common underlying diseases in patients were hypertension (15%) and diabetes (9.5%). Other underlying diseases were cardiovascular diseases (7.75%), lung disease (4.2%), and cancer (3.25%). The prevalence of underlying diseases was higher in the deceased cases than in the recovered patients, and this difference was statistically significant. This finding is consistent with the results of Najafi et al. [23]. They assessed the clinical characteristics of 214 COVID-19 patients who died in a hospital in Sari City, north of Iran. The most common underlying diseases in patients were hypertension (47.2%), cardiovascular disease (45.8%), and diabetes (40.7%). In Zali et al.’s study, the deceased cases in Tehran had diabetes and cardiovascular diseases (38.46%) and cancer (35.79%) [14]. As can be seen, the prevalence of underlying diseases is higher in these studies conducted in the north of Iran compared to our research conducted in the west of Iran. In Sheikhi et al.’s study in the south of Iran, hypertension was reported in 24.3%, heart disease in 22.5%, and diabetes in 12.4% of hospitalized patients [16]. Nouri-Vaskeh et al. also noted that diabetes, hypertension, and cardiovascular diseases were more common among the deceased COVID-19 patients in northwest Iran [15]. Grasselli et al. also reported that chronic obstructive pulmonary disease, hypercholesterolemia, and type 2 diabetes were risk factors associated with mortality from COVID-19 in Italy [12].
Regarding the laboratory findings, the difference between the deceased and recovered groups in our study was statistically significant in terms of WBC count and neutrophil percentage, as well as Cr and K levels, where the deceased patients had higher values in these variables. We found no significant difference between the deceased and recovered groups in ESR, eosinophil percentage, lymphocyte percentage, AST, ALT, ALP, or BUN. These results are consistent with Mehri et al.’s findings regarding WBC count and Cr level but are against their results regarding lymphocyte percentage and BUN. They reported a significant association between increased WBC count, decreased lymphocyte, and increased BUN with death from COVID-19 [1]. In Haghighi et al.’s study in the north of Iran, the increase in neutrophil and lymphopenia percentages and the ESR are the most common laboratory findings in COVID-19 patients admitted to ICU [18]. In Talebi et al.’s study in northeast Iran, increased WBC count decreased lymphocyte percentage, and increased neutrophil percentage were significantly higher in deceased COVID-19 patients [17]. Their results are in agreement with our findings, except for lymphocyte percentage. Ghelmani et al. also reported the relationship of increased WBC count with death by COVID-19 in patients admitted to a hospital in Yazd City, central Iran [19].
This study was the first to investigate the clinical and laboratory characteristics of COVID-19 patients in Khorramabad, western Iran. However, it had some limitations, such as the short duration of the study (6 months) and the incompleteness of some medical records regarding the demographic, clinical, and laboratory data. Due to the higher rate of COVID-19 infection and death in older people, those with underlying diseases, as well as smokers, control and preventive measures are necessary in these groups. Since cough and shortness of breath are the most frequent symptoms among patients with COVID-19, paying attention to these symptoms at the time of admission to the hospital helps identify and predict infected patients.
Conclusion
Shortness of breath, dry cough, nausea/vomiting, and anorexia were the most prevalent clinical symptoms in patients with COVID-19 admitted to an educational hospital in Khorramabad City. The most common underlying diseases in these patients were hypertension and diabetes. The death rate due to COVID-19 was higher among older, married, and unemployed patients and those with higher WBC count, neutrophil percentage, and creatinine and potassium levels.
Ethical Considerations
Compliance with ethical guidelines
In this study, all ethical principles were considered. The study was approved by the Ethics Committee of Lorestan University of Medical Sciences (Code: IR.LUMS.REC.1401.022).
Funding
This study was extracted from the PhD dissertation of Zahra Vaez, approved by the Department of Social Medicine, School of Medicine, Lorestan University of Medical Sciences. It was not funded by any organization.
Authors' contributions
Study design, methodology, data collection, and writing the original draft: Zahra Vaez; Supervision, data analysis, project administration, editing, and review: Parastoo Baharvand; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the staff of Shahadaye Ashayer Hospital for their cooperation in this study.
References
In December 2019, the new coronavirus (COVID-19) was detected in Wuhan, China and spread rapidly worldwide. It affected the health systems and created a global health crisis. Iran’s Ministry of Health and Medical Education officially announced that two people in Qom City were infected with COVID-19 on February 19, 2020. This number later increased dramatically, and the disease spread to other parts of Iran. Studies on the course of the disease show that control and preventive measures significantly reduce the prevalence of COVID-19 and its mortality. Many studies have been conducted to investigate the risk factors affecting the death or recovery of patients with COVID-19 in Iran and other countries to provide comprehensive information in the field of treatment and control [1-12]. Mehri et al., in a systematic meta-analysis study, reported a significant association between death from COVID-19 and age, male gender, diabetes, hypertension, cardiovascular disease, cerebrovascular disease, chronic kidney disease, headache, and dyspnea. Moreover, they found a significant association between increased white blood cell (WBC), decreased lymphocytes, increased blood urea nitrogen (BUN), increased creatinine (Cr), vitamin D deficiency, and death from COVID-19 [1]. Arman et al., in a study on patients with COVID-19 in Tehran, Iran, reported that cough, respiratory distress, and fever were the most common symptoms of COVID-19. In their research, cancer, chronic lung diseases, and chronic neurologic diseases were the strongest risk factors for death in COVID-19 patients [8]. In Jalili et al.’s national cohort study on 28981 hospitalized patients with COVID-19 from 1034 hospitals in Iran, heart disease, asthma, chronic obstructive pulmonary disease, chronic kidney disease, cancer, and chronic liver disease had an association with death in patients with COVID-19 [13]. In Zali et al.’s study on 16016 hospitalized patients with COVID-19 in Tehran City, Iran, the highest total death rate was observed in patients aged >65 years (25.32%) with diabetes and cardiovascular diseases (38.46%), and cancer (35.79%) [14]. Nouri-Vaskeh et al. investigated the characteristics of 111 patients who died of COVID-19 in Tabriz City, northwest of Iran. According to their studies, dyspnea, cough, and fever were the most common symptoms. Among comorbidities, diabetes, hypertension, and cardiovascular diseases were more common among the deceased patients [15]. Sheikhi et al. assessed the demographic and clinical characteristics of 169 hospitalized patients with COVID-19 in Iranshahr, southeast of Iran. In their study, a history of hypertension was reported in 24.3%, heart disease in 22.5%, and diabetes in 12.4% of patients. Shortness of breath with 71.6% and cough with 69.8% were the most common symptoms, while chest pain with 7.7% was the least common. Of 169 patients, 146(86.4%) recovered, and 34(13.6%) died [16]. Talebi et al. compared the clinical and epidemiological characteristics of deceased and recovered patients with COVID-19 in Sabzevar, northeast of Iran. Of 178 patients, 85.4% recovered, and 14% died. Shortness of breath (72.5%) was the most common symptom, followed by cough (61.8%) and fever (48.9%). Moreover, 43.8% of all patients and 71.9% of deceased patients had at least one underlying disease. Increased WBC count, decreased lymphocyte, and increased neutrophils were significantly higher in deceased cases [17]. Haghighi et al. investigated the demographic, clinical, laboratory characteristics, and imaging features of patients with COVID-19 admitted to the intensive care unit (ICU) of hospitals in Rasht City, Northern Iran. Diabetes mellitus, hypertension, and chronic heart disease were the most common underlying diseases. Shortness of breath, fever, and cough were the most common symptoms. Ground-glass opacity was the most common lung CT scan finding, and an increase in the level of lactate dehydrogenase (LDH), erythrocyte sedimentation rate (ESR), C-reactive protein rate, neutrophil percentage, and lymphopenia were the most common laboratory findings in the patients. The mortality rate was 90.58% [18]. Ghelmani et al. investigated the risk factors associated with mortality in 932 patients with COVID-19 admitted to a hospital in Yazd, central Iran. The mortality rate was 9.6% (n=82). The identified risk factors were higher age, shortness of breath, history of cancer, hospitalization in the ICU, increased WBC count, and sodium deficiency [19].
Exploring the epidemiological features of COVID-19 and assessing underlying comorbidities among affected patients could help public health officials, decision-makers, and clinicians take the initiative in reducing the burden of this infectious disease and consequently controlling the pandemic. Although several studies have been recently performed to report specific epidemiological and clinical characteristics of COVID-19 patients in Iran, we found no study on the characteristics of hospitalized patients in Khorramabad, western Iran. In this regard, this epidemiological study aims to investigate the demographic, clinical, and laboratory characteristics of patients with COVID-19 admitted to a hospital in Khorramabad city to find the factors associated with death from COVID-19.
Materials and Methods
This research is a descriptive-analytical study with a cross-sectional design. The data of all patients with COVID-19 hospitalized in an educational hospital (Shahadaye Ashayer) affiliated with Lorestan University of Medical Sciences in the mid-year of 2021 were examined (n=555). The inclusion criteria were a definite diagnosis of COVID-19 (RT-PCR positive) and hospitalization in special units for coronavirus cases. The exclusion included the definite diagnosis of other respiratory diseases, flu, and respiratory problems unrelated to COVID-19 and incomplete medical files.
A researcher-made checklist was used to extract patients’ information, including demographic information (age, sex, occupation, educational level, marital status, place of residence), history of smoking, clinical symptoms, history of underlying diseases, and laboratory findings. The data were collected from the patient’s medical files by referring to the hospital’s medical data archive system. Then, they were analyzed in SPSS software, version 19, using descriptive statistics, independent t-test, and chi-square test. The significance level was set at 0.05.
Results
Among 555 patients, 295(53.1%) were male and 260(46.9%) were female. There were 481 recovered cases (86.7%) and 74 deceased cases (13.3%). The mean age of patients was 58.49±13.25 years, where recovered cases had a mean age of 55.08±10.91 years (range: 17-82 years), and the deceased cases had a mean age of 77.18±9.46 years (range: 56-87 years). According to the independent t-test results, the difference between the two groups regarding age was statistically significant (P<0.001). Most patients were married (n=419, 75.4%) with high school diplomas (n=223, 40.2%) and were living in urban areas (n=500, 90.2%) with no history of smoking (n=334, 60.2%). The personal characteristics of the patients in the deceased and recovered groups are presented in Table 1.
The results of the chi-square test showed that the differences between the two groups were statistically significant in terms of marital status (P=0.001), occupation (P=0.001), and history of smoking (P=0.002). No significant difference was found in terms of sex and place of residence (P>0.05) (Table 1).
Regarding the clinical findings (Figure 1), the prevalence rates of fever and muscle pain (systemic symptoms) were 36.3% (n=202) and 35.3% (n=196), respectively. The prevalence of shortness of breath and dry cough (pulmonary symptoms) was 74.2% (n=412) and 63.2% (n=351), respectively. The prevalence of nausea/vomiting and anorexia (gastrointestinal symptoms) was 56.6% (n=314) and 57.2% (n=318), respectively. Chest pain had a low prevalence rate of 9.5% (n=53). The results of the chi-square test showed that the differences between the two groups were significant in terms of all clinical symptoms (P<0.05) (Table 2).
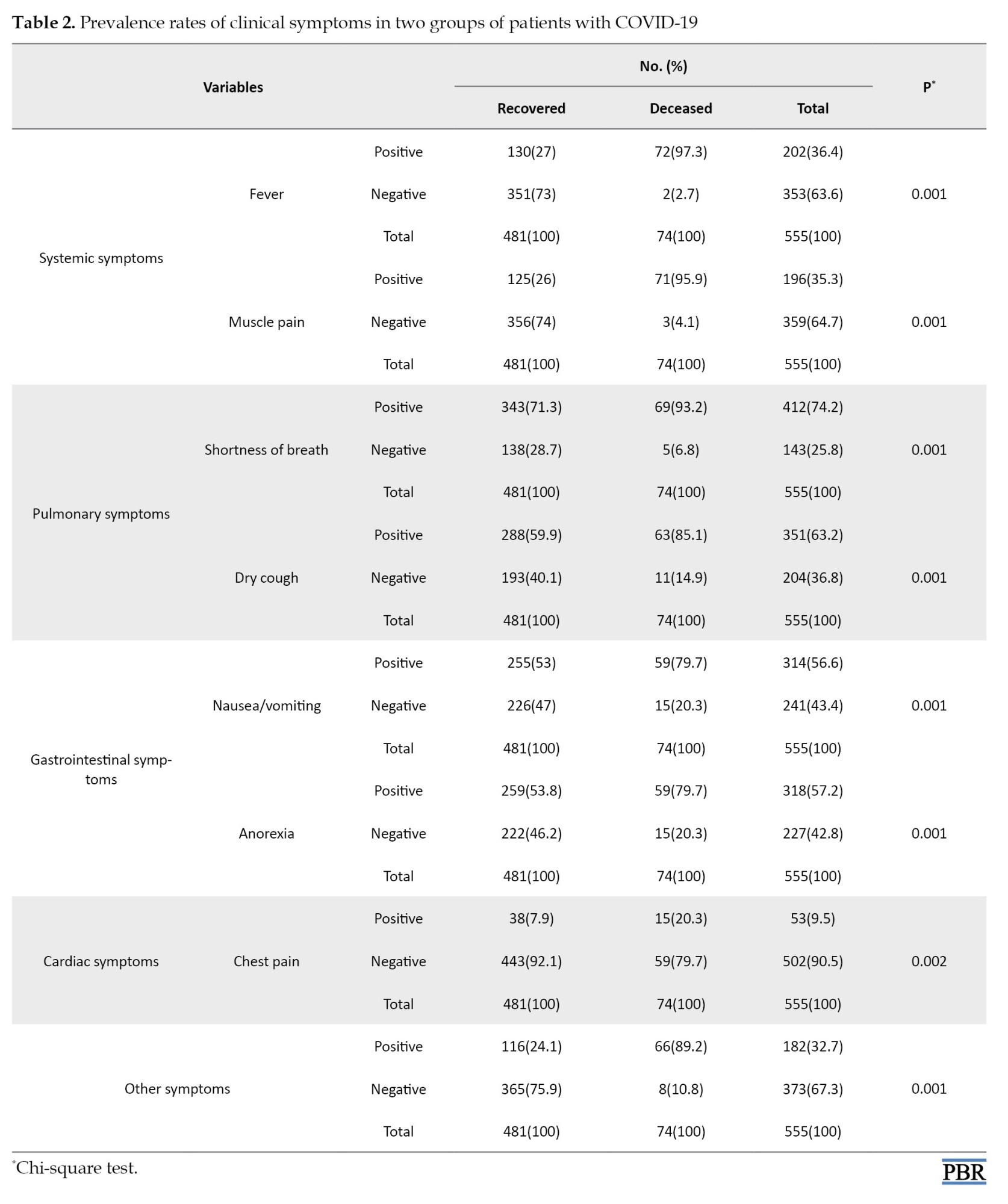
Regarding the laboratory findings, the means of WBC count, platelet count, and ESR in COVID-19 patients were 11.2±1.6 (×109/L), 250.13±98.18 (×109/L), and 82.25±2.3 (mm/h), respectively. The mean percentages of neutrophils, eosinophils, and lymphocytes (the components of WBCs) were 71.3±2.06%, 1.03±0.5%, and 25.03±1.07%. The mean levels of Cr, potassium (K), sodium (Na), and BUN were 2.01±0.01, 3.8±0.5, 137.7±1.08, and 32.7±4.08, respectively. Moreover, the mean levels of liver enzymes aspartate transaminase (AST), alkaline transaminase (ALT), and alkaline phosphatase (ALP) were 37.58±10.16, 36.43±9.24, and 181.04±93.99 (U/L), respectively. The laboratory findings of the patients for the deceased and recovered groups are presented in Table 3.
According to the results of the independent t-test, the difference between the recovered and deceased groups was statistically significant only in terms of WBC count (P=0.049; 10.81±2.1 vs 12.36±2.2), neutrophil percentage (P=0.009; 70.74±6.5% vs 72.91±7.03%), Cr level (P=0.001; 1.08±0.25 vs 1.2±0.53 mg/dL), and K level (P=0.037; 3.5±0.29 vs 3.6±0.4 mEq/L).
Regarding the underlying diseases, it was found that 103 out of 555 patients with COVID-19 had underlying diseases, 23(4.2%) had lung disease, 83(15%) hypertension, 53(9.5%) diabetes, 43(7.75%) cardiovascular diseases, 18(3.25%) cancer, and 20(3.6%) reported other diseases. Table 4 presents the frequency of underlying diseases for each group of deceased and recovered cases.
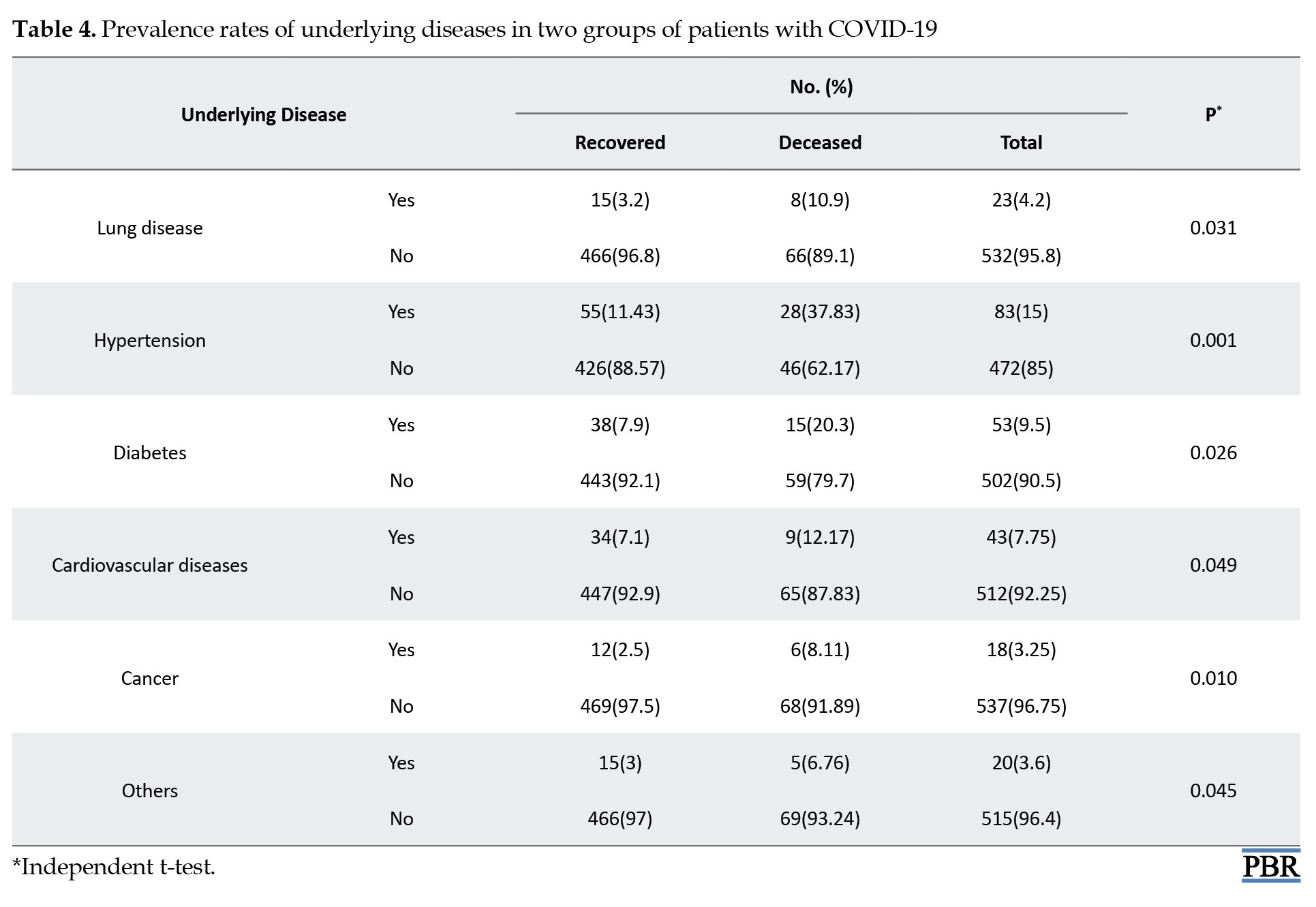
As can be seen, the frequency of underlying diseases was higher in the deceased cases than in the recovered patients, and this difference was significant in all underlying diseases (P<0.05).
Discussion
This study aimed to investigate the epidemiological and clinical characteristics of patients with COVID-19 admitted to a hospital in Khorramabad, Iran. The data of 555 patients were examined. The prevalence of mortality was reported 13.3% (n=74). This number is close to the prevalence rates reported by Sheikhi et al. (13.6%) in Iranshahr City and Talebi et al. (14%) in Sabzevar City [16-17] but lower than the death rate reported by Haghighi et al. (90.58%) on ICU patients in Rasht City [18], and higher than the rate reported by Ghelmani et al. (9.6%) in Yazd City [19]. In Grasselli et al.’s study in a city in Italy of 3988 hospitalized patients with COVID-19, the mortality rate was reported 915(53.4%) in the hospital [12]. This number is higher than the prevalence rate reported in our study. The difference in the mortality rates may be due to the difference in the disease severity in the studied patients and the quality of medical care provided by the studied hospitals.
In our study, the deceased patients had a mean age of 77.18±9.46 years (range: 56-87 years) and were older than the recovered cases with a mean age of 55.08±10.91 years. This difference was statistically significant. This finding is consistent with the results of previous studies in Iran [14, 16-19] and other countries [12], which reported that old age is a risk factor for death by COVID-19 in hospitalized patients. Another finding was that the death rate was significantly higher in hospitalized patients with a history of smoking tobacco (56.8%). Smoking can reduce the function of the immune system and is associated with a decrease in the number and proportion of circulating natural killer cells [ 20]. In a review study, Vardavas and Nikitara reported that smokers showed 1.4 times more severe symptoms of COVID-19 and approximately 2.4 times more likely to be admitted to ICU. They need more mechanical ventilation and die compared to non-smokers [21].
In this study, shortness of breath, dry cough, nausea/vomiting, and anorexia were the most prevalent clinical symptoms in patients with COVID-19, while chest pain had the lowest prevalence. All clinical symptoms were significantly related to the death of COVID-19. These results are consistent with the reports of Nouri-Vaskeh et al., Sheikhi et al., Talebi et al., Haghighi et al., and Gozidehkar et al. for hospitalized COVID-19 patients in other parts of Iran [15-18, 22]. In our study, the most common underlying diseases in patients were hypertension (15%) and diabetes (9.5%). Other underlying diseases were cardiovascular diseases (7.75%), lung disease (4.2%), and cancer (3.25%). The prevalence of underlying diseases was higher in the deceased cases than in the recovered patients, and this difference was statistically significant. This finding is consistent with the results of Najafi et al. [23]. They assessed the clinical characteristics of 214 COVID-19 patients who died in a hospital in Sari City, north of Iran. The most common underlying diseases in patients were hypertension (47.2%), cardiovascular disease (45.8%), and diabetes (40.7%). In Zali et al.’s study, the deceased cases in Tehran had diabetes and cardiovascular diseases (38.46%) and cancer (35.79%) [14]. As can be seen, the prevalence of underlying diseases is higher in these studies conducted in the north of Iran compared to our research conducted in the west of Iran. In Sheikhi et al.’s study in the south of Iran, hypertension was reported in 24.3%, heart disease in 22.5%, and diabetes in 12.4% of hospitalized patients [16]. Nouri-Vaskeh et al. also noted that diabetes, hypertension, and cardiovascular diseases were more common among the deceased COVID-19 patients in northwest Iran [15]. Grasselli et al. also reported that chronic obstructive pulmonary disease, hypercholesterolemia, and type 2 diabetes were risk factors associated with mortality from COVID-19 in Italy [12].
Regarding the laboratory findings, the difference between the deceased and recovered groups in our study was statistically significant in terms of WBC count and neutrophil percentage, as well as Cr and K levels, where the deceased patients had higher values in these variables. We found no significant difference between the deceased and recovered groups in ESR, eosinophil percentage, lymphocyte percentage, AST, ALT, ALP, or BUN. These results are consistent with Mehri et al.’s findings regarding WBC count and Cr level but are against their results regarding lymphocyte percentage and BUN. They reported a significant association between increased WBC count, decreased lymphocyte, and increased BUN with death from COVID-19 [1]. In Haghighi et al.’s study in the north of Iran, the increase in neutrophil and lymphopenia percentages and the ESR are the most common laboratory findings in COVID-19 patients admitted to ICU [18]. In Talebi et al.’s study in northeast Iran, increased WBC count decreased lymphocyte percentage, and increased neutrophil percentage were significantly higher in deceased COVID-19 patients [17]. Their results are in agreement with our findings, except for lymphocyte percentage. Ghelmani et al. also reported the relationship of increased WBC count with death by COVID-19 in patients admitted to a hospital in Yazd City, central Iran [19].
This study was the first to investigate the clinical and laboratory characteristics of COVID-19 patients in Khorramabad, western Iran. However, it had some limitations, such as the short duration of the study (6 months) and the incompleteness of some medical records regarding the demographic, clinical, and laboratory data. Due to the higher rate of COVID-19 infection and death in older people, those with underlying diseases, as well as smokers, control and preventive measures are necessary in these groups. Since cough and shortness of breath are the most frequent symptoms among patients with COVID-19, paying attention to these symptoms at the time of admission to the hospital helps identify and predict infected patients.
Conclusion
Shortness of breath, dry cough, nausea/vomiting, and anorexia were the most prevalent clinical symptoms in patients with COVID-19 admitted to an educational hospital in Khorramabad City. The most common underlying diseases in these patients were hypertension and diabetes. The death rate due to COVID-19 was higher among older, married, and unemployed patients and those with higher WBC count, neutrophil percentage, and creatinine and potassium levels.
Ethical Considerations
Compliance with ethical guidelines
In this study, all ethical principles were considered. The study was approved by the Ethics Committee of Lorestan University of Medical Sciences (Code: IR.LUMS.REC.1401.022).
Funding
This study was extracted from the PhD dissertation of Zahra Vaez, approved by the Department of Social Medicine, School of Medicine, Lorestan University of Medical Sciences. It was not funded by any organization.
Authors' contributions
Study design, methodology, data collection, and writing the original draft: Zahra Vaez; Supervision, data analysis, project administration, editing, and review: Parastoo Baharvand; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the staff of Shahadaye Ashayer Hospital for their cooperation in this study.
References
- Mehri A, Sotoodeh Ghorbani S, Farhadi-Babadi K, Rahimi E, Barati Z, Taherpour N, et al. Risk factors associated with severity and death from covid-19 in Iran: A systematic review and meta-analysis study. J Intensive Care Med. 2023; 38(9):825-37. [DOI:10.1177/08850666231166344] [PMID]
- Dadgari A, Mirrezaei SM, Talebi SS, Alaghemand Gheshlaghi Y, Rohani-Rasaf M. [Investigating some risk factors related to the covid-19 pandemic in the middle-aged and elderly (Persian)]. Salmand Iran J Ageing. 2021; 16(1):102-11. [DOI:10.32598/sija.16.1.3172.1]
- Martono, Fatmawati F, Mulyanti S. Risk factors associated with the severity of covid-19. Malays J Med Sci. 2023; 30(3):84-92. [DOI:10.21315/mjms2023.30.3.7] [PMID]
- Zhang JJ, Dong X, Liu GH, Gao YD. Risk and protective factors for covid-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. 2023; 64(1):90-107. [DOI:10.1007/s12016-022-08921-5] [PMID]
- Zhong R, Chen L, Zhang Q, Li B, Qiu Y, Wang W, et al. Which factors, smoking, drinking alcohol, betel quid chewing, or underlying diseases, are more likely to influence the severity of COVID-19? Front Physiol. 2021; 11:623498. [DOI:10.3389/fphys.2020.623498] [PMID]
- Borjas GJ. Demographic determinants of testing incidence and COVID-19 infections in New York City neighborhoods. Nat Bureau Econ Res. 2021; 0898-2937. [Link]
- Jorjoran Shushtari Z, Shirazikhah M, Ahmadi S, Salimi Y, Biglarian A, Almasi A. Upstream determinants and downstream risk factors of covid-19 infection in Iran: A qualitative study of health professionals’ views. J Health Sci Surveill Syst. 2022; 10(3):365-75. [DOI:10.30476/jhsss.2021.92017.1290]
- Arman A, Tajik M, Nazemipour M, Ahmadinejad Z, Shahrestanaki SK, Hazrati E, et al. Risk factors of developing critical conditions in Iranian patients with COVID-19. Glob Epidemiol. 2021; 3:100046. [DOI:10.1016/j.gloepi.2020.100046] [PMID]
- Huang K, Zhang J, Wu W, Huang D, He C, Yang Y, et al. A retrospective analysis of the epidemiology, clinical manifestations, and imaging characteristics of familial cluster-onset COVID-19. Ann Transl Med. 2020; 8(12):747. [DOI:10.21037/atm-20-3759] [PMID]
- Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol. 2020; 55(5):1169-74. [DOI:10.1002/ppul.24718] [PMID]
- Huang C, Wang Y, Li X, Ran L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497-506. [DOI:10.1016/S0140-6736(20)30183-5] [PMID]
- Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020; 180(10):1345-55.[DOI:10.1001/jamainternmed.2020.3539] [PMID]
- Jalili M, Payandemehr P, Saghaei A, Sari HN, Safikhani H, Kolivand P. Characteristics and mortality of hospitalized patients with covid-19 in Iran: A national retrospective cohort study. Ann Intern Med. 2021; 174(1):125-27. [DOI:10.7326/M20-2911] [PMID]
- Zali A, Gholamzadeh S, Mohammadi G, Azizmohammad Looha M, Akrami F, Zarean E, et al. Baseline characteristics and associated factors of mortality in covid-19 patients; an analysis of 16000 cases in Tehran, Iran. Arch Acad Emerg Med. 2020; 8(1):e70. [PMID]
- Nouri-Vaskeh M, Khalili N, Sharifi A, Behnam P, Soroureddin Z, Ade EA, et al. Clinical characteristics of fatal cases of COVID-19 in Tabriz, Iran: An analysis of 111 patients. Front Emerg Med. 2020; 5(1):e12. [Link]
- Sheikhi F, Mirkazehi Rigi Z, Azarkish F, Kalkali S, Seid Abadi M, Mirbaloochzehi A. [Clinical and demographic characteristics of patients with COVID-19 in Iranshahr Hospitals, southeastern Iran in 2020 (Persian)]. J Mar Med. 2021; 3(1):46-52. [DOI:10.30491/3.1.46]
- Talebi S, Nematshahi M, Tajabadi A, Khosrogerdi A. [Comparison of clinical and epidemiological characteristics of deceased and recovered patients with COVID-19 in Sabzevar, Iran (Persian)]. J Mil Med. 2020; 22(6):509-16. [DOI:10.30491/JMM.22.6.509]
- Haghighi M, Khoshrang H, Ghazanfar Tehran S, Aghajanzadeh P, Jafarinezhad A, Souri Z, et al. [Evaluation of epidemiological, paraclinical, and imaging findings of patients with covid-19 hospitalized in Intensive Care Unit of Rasht Hospitals in March 2020 (Persian)]. J Guilan Univ Med Sci. 2021; 30(2):84-97. [DOI:10.32598/JGUMS.30.2.1619.2]
- Ghelmani SY, Salehabadi HS, Moazen H, Nazmiah H, Tafti T, Kabirzadeh A, et al. [Evaluation of risk factors related to life status of patients with covid-19 hospitalized in Yazd (Persian). J Tolooebehdasht. 2022; 21(2):85-98. [DOI:10.18502/tbj.v21i2.10343]
- Tollerud DJ, Clark JW, Brown LM, Neuland CY, Mann DL, Pankiw-Trost LK, et al. Association of cigarette smoking with decreased numbers of circulating natural killer cells. Am Rev Respir Dis. 1989; 139(1):194-8. [DOI:10.1164/ajrccm/139.1.194] [PMID]
- Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis. 2020; 18:20. [DOI:10.18332/tid/119324] [PMID]
- Gozidehkar Z, Gahani H, Davary A, Borna H. [Prevalence and factors related to infection and mortality due to COVID-19 among patients of Shohada Ghaen Hospital, Ghaen, Iran, 2020 (Persian)]. J Birjand Univ Med Sci. 2021 ; 28(4):375-84. [DOI:10.32592/JBirjandUnivMedSci.2021.28.4.106]
- Najafi N, Bakhshi P, Alizadeh- Navaei R, Ahangarkani F, Akbari Z, Mirzakhani M et al. [Clinical epidemiology of deceased covid-19 patients in Mazandaran Heart Center, 2020-2021 (Persian)]. J Mazandaran Univ Med Sci. 2022; 32 (207):79-89. [Link]
Type of Study: Original Research |
Subject:
General
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |