Volume 9, Issue 4 (2023)
Pharm Biomed Res 2023, 9(4): 321-324 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kargar-soleimanabad S, Gholitabaromrani R, Gholami F. Acute Kidney Injury and Rhabdomyolysis Following Multi-drug Suicide Attempt: A Case Report. Pharm Biomed Res 2023; 9 (4) :321-324
URL: http://pbr.mazums.ac.ir/article-1-564-en.html
URL: http://pbr.mazums.ac.ir/article-1-564-en.html
1- Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Internal Medicine, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Internal Medicine, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 494 kb]
(620 Downloads)
| Abstract (HTML) (1802 Views)
References
Full-Text: (542 Views)
Introduction
Acute kidney injury (AKI), known as acute renal failure, refers to a sudden and irreversible decrease in overall kidney function over hours to days, resulting in the body’s inability to control electrolyte balance, water, acid, and base [1]. AKI is usually assessed by measuring glomerular filtration rate (GFR) and increased levels of creatinine, in addition to blood urea nitrogen and fractional sodium excretion in some cases. The exact prevalence of AKI in the general population is unknown; however, studies have shown a 7% prevalence in hospitalized patients and 30% in ICU patients, indicating that a large number of patients admitted to medical and ICU wards, as well as non-hospitalized patients are at risk for AKI [2]. This high prevalence reflects AKI as a serious challenge for healthcare systems. An increase in complications usually accompanies the occurrence of AKI, the possibility of progression to chronic kidney disease (CKD), as well as short-term and long-term mortality. Patients requiring dialysis and renal replacement therapy have about 50 times higher chances of progressing toward chronic kidney diseases [3].
AKI is a complex clinical syndrome classified into the following three categories based on the anatomical site of involvement: Prerenal, intrinsic renal, and postrenal. AKI with intrinsic origin is classified based on the site of involvement in the kidney, which includes tubules, glomeruli, renal vessels, and interstitial tissue. Causes of intrinsic injury include prolonged hypo-perfusion, sepsis, and nephrotoxins. These toxins can originate from within the body, such as hemoglobin and myoglobin, or from outside the body, such as drugs like aminoglycosides, vancomycin, amphotericin, and pentamidine [4].
Rhabdomyolysis is a clinical event characterized by muscle damage, disruption of muscle fibers, and release of intracellular contents into the bloodstream. Myoglobin, creatine phosphokinase, and lactate dehydrogenase are among the main intracellular contents of muscle that are used to assess the extent of damage [5]. The most common clinical manifestations of rhabdomyolysis are myalgia, fatigue, red-colored urine, and swelling in the affected muscle; however, it can also present with less common and nonspecific symptoms, such as fever, nausea, vomiting, and dyspnea. The leading causes of rhabdomyolysis include trauma, drugs such as statins, toxins, temperature extremes, excessive physical activity, and inherited and acquired metabolic disorders in the muscle [6].
Case Presentation
A 40-year-old male patient was transferred to the emergency department by EMS with complaints of decreased consciousness. The patient reported ingesting 40 tablets of 20 mg methadone, 27 tablets of 10 mg nortriptyline, and 13 tablets of 2 mg clonazepam three days before admission. He had been in his room for the past three days and had not eaten or urinated. In terms of medical history, the patient had a history of addiction and had been on daily methadone treatment for 20 days, which he stopped two months ago. He also mentioned several unsuccessful suicide attempts with methadone. His past psychiatry history included major depression disorder and substance abuse for more than ten years.
On initial examination, the patient weighed approximately 70 kg, had a blood pressure of 85/60, a heart rate of 70 beats per minute, a respiratory rate of 15 breaths per minute, and a Glasgow coma scale score of 10. The patient had extensive erythema on the right side of his body, which was caused by prolonged lying on that side. The erythema involved the right arm, right side of the body, and right leg. The patient confirmed that he had been lying in this position for two days without changing. There were also blisters on the posterior aspect of the shoulder joint, the forearm, and the right side of the patient’s body. Due to decreased consciousness and drowsiness, the patient could not express his main complaint; however, weakness and muscle pain, especially on the right side of the body, were apparent on physical examination.
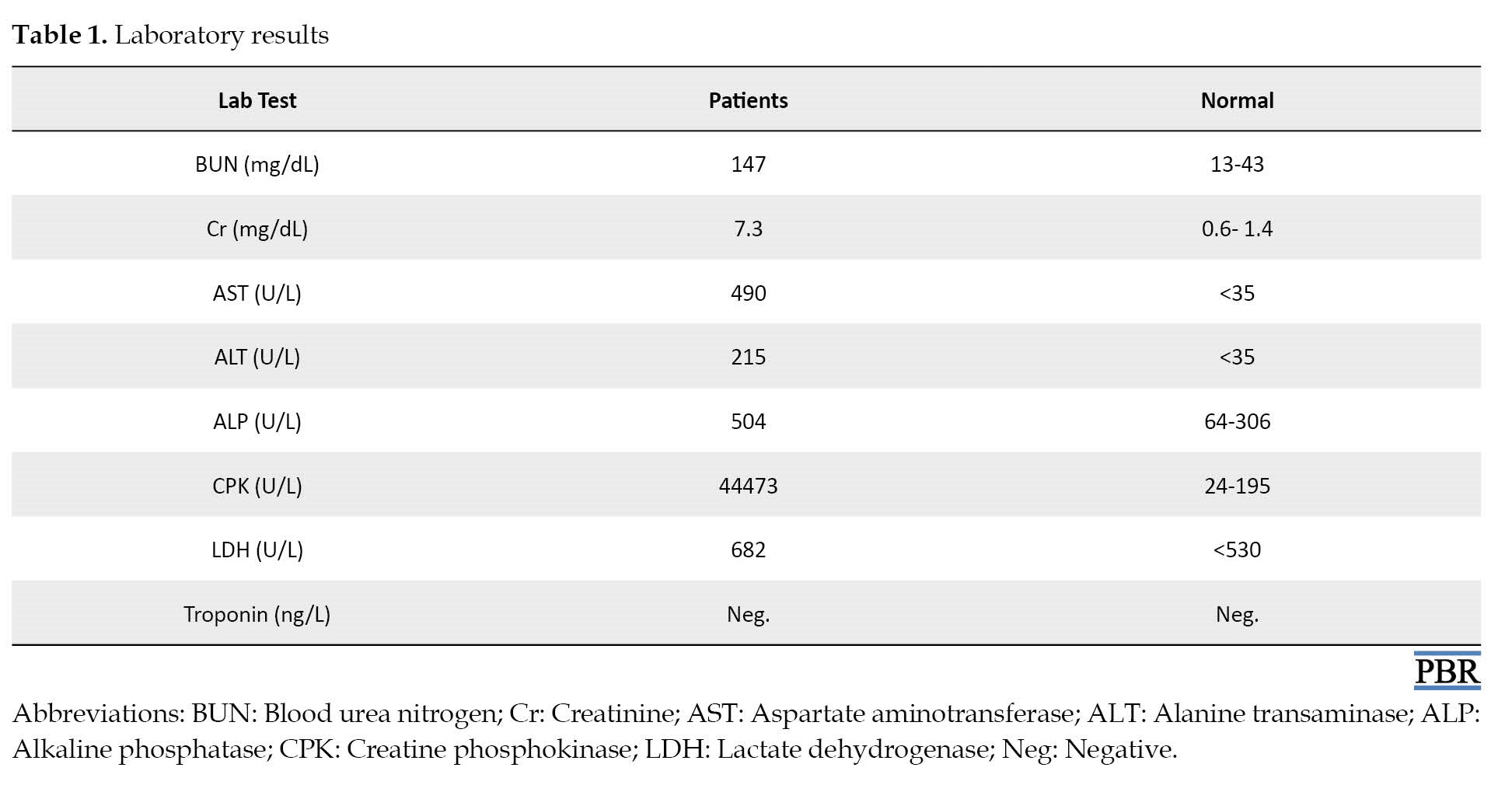
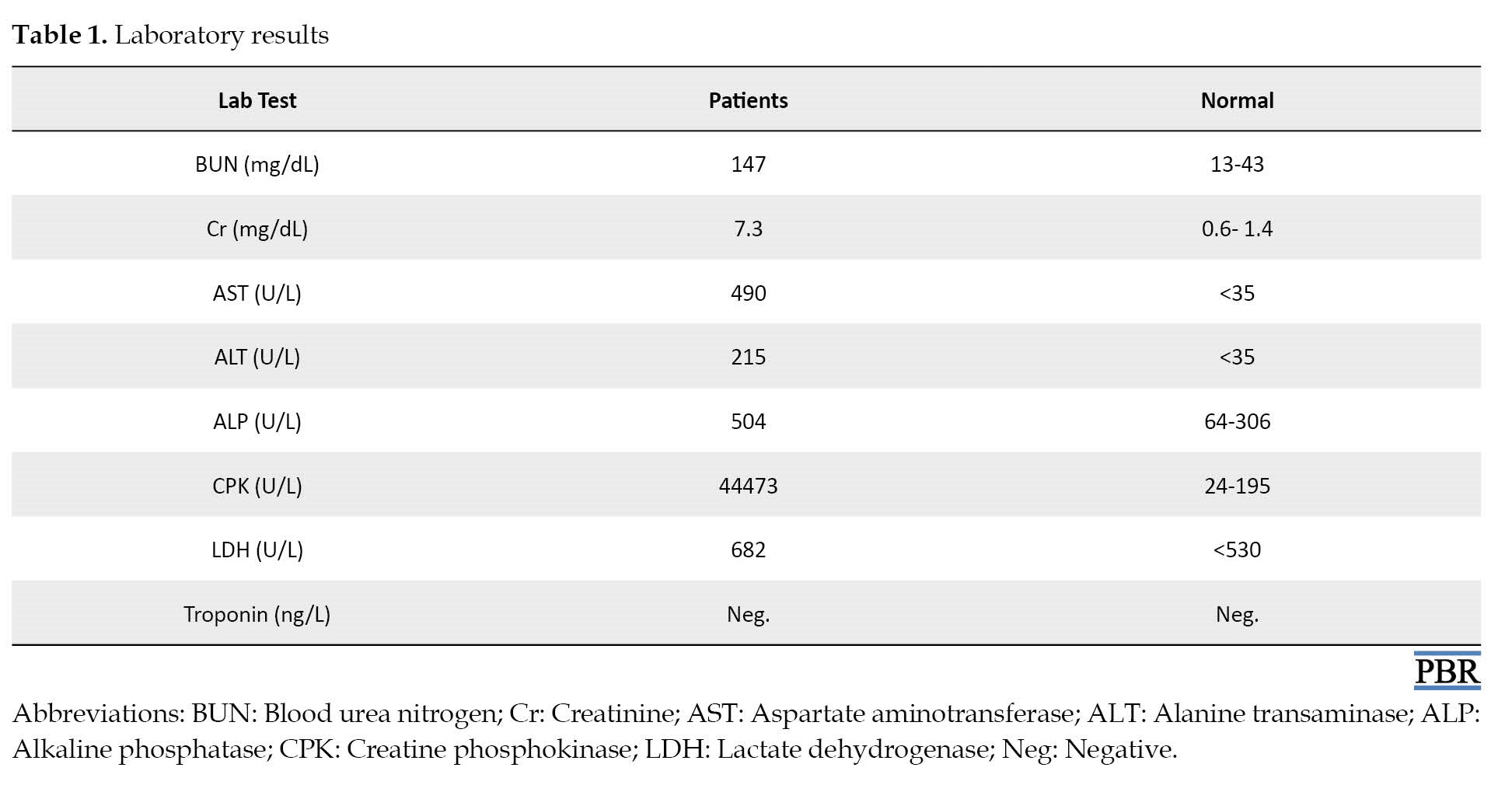
Complete laboratory tests, electrocardiogram, and toxicology consult were requested for the patient; laboratory tests showed respiratory acidosis partially compensated by metabolic alkalosis. The patient had increased creatinine levels, liver enzymes (aspartate transaminase approximately 14 times normal, alanine transaminase approximately six times normal), and creatine phosphokinase-MB (approximately 230 times normal; Table 1).
Based on the clinical symptoms, AKI following rhabdomyolysis was suspected in the patient, which was confirmed by laboratory results. As the first step, intravenous hydration was initiated for the patient, and fluid intake and output were monitored. Kidney function tests, electrolytes, and daily consultations with toxicology were requested for the patient. One day after treatment, the respiratory acidosis was corrected, and on the fourth day of hospitalization, the patient’s creatinine level returned to 1.2 mg/dL, which was in the normal range. The patient was discharged with a good general condition.
Discussion
Some commentators define the term “suicidal behaviors” as a general term that encompasses all thoughts and actions related to suicide without distinguishing between thoughts and plans, non-lethal acts, and acts that result in death. Suicide is now recognized as one of the leading causes of death, morbidity, and disability worldwide. The level of effort and success in suicide attempts varies depending on different circumstances; however, epidemiological studies have shown that age, gender, socioeconomic status, geographical location, and country of residence have an impact on the rate of suicide attempts and their success [7]. Among these factors, the rate of suicide attempts is higher in older individuals, and mortality rates are higher in males, with suicide attempts in women being twice as high as in men. However, the methods used by women are less lethal, and the mortality and success rates in completing suicide are higher in older individuals. Different individuals choose different suicide methods based on their circumstances and preferences. However, methods such as hanging, using firearms, suffocation, jumping from heights, and drug poisoning are the most common and widely used methods of suicide [8]. The simultaneous use of multiple methods for suicide is referred to as “complex suicide.” In some cases of complex suicide, an individual may use multiple drugs, and the simultaneous use of multiple drugs with different pharmacokinetics and pharmacodynamics can affect the course of the disease and the effectiveness of therapeutic interventions [9]. Suicide attempts are often carried out using drugs, with benzodiazepines, antipsychotics, barbiturates, and antidepressants having the highest rates of use. According to many studies, benzodiazepines are used for suicide along with other drugs that have suppressive effects on the nervous system [10]. In the present case study, a 40-year-old male patient with a previous history of suicide attempts presented to the emergency department after ingesting methadone, clonazepam, and nortriptyline.
Methadone is a fully synthetic opioid with a long duration of action that is similar to morphine but does not have the same potency. Similar to other opioids, this drug binds to opioid receptors on the surface of cells in the central nervous system, lungs, heart, blood vessels, and intestines and has a similar mechanism of action. Therefore, the high dosage of this drug can cause symptoms of central nervous system and respiratory suppression, leading to decreased consciousness, sedation, and bradypnea. On the other hand, the patient in this study had consumed a significant amount of clonazepam, which, when used concurrently with opioids, can exacerbate respiratory and nervous system suppression [11]. Predictably, without antidote use, the patient would experience decreased levels of consciousness and sedation for approximately 48 h. Additionally, the patient had consumed an excessive amount of nortriptyline, which can also cause reduced consciousness, muscle involvement, and muscle stiffness as symptoms of toxicity. Considering this drug overdose in a complex manner in this patient, it was expected that he would experience decreased levels of consciousness and sedation for approximately 48 h. Furthermore, due to the patient’s companions not paying attention to his prolonged sleep, lack of movement, and failure to change position during the intoxication period, rhabdomyolysis was suspected based on the patient’s clinical symptoms, including extensive erythema on the right side and pain on palpation [12]. Laboratory results confirmed this diagnosis. Considering that rhabdomyolysis and the release of intracellular contents such as myoglobin can cause damage to kidney tissue and lead to AKI. A workup for AKI was performed for the patient. With early treatment initiation, the extent of kidney damage did not progress, and the patient’s creatinine level did not exceed 1.6, resulting in a stable condition.
Although direct drug poisoning did not cause death or organ damage in this case, the decrease in consciousness level, which is one of the main adverse effects of benzodiazepine and opioid poisoning, can create favorable conditions for events such as rhabdomyolysis, aspiration pneumonia, etc. leading to irreversible complications. In some cases, these complications may be more harmful than the risks associated with suicidal behaviors themselves.
Conclusion
The toxic effects lead to the creation of conditions that, although not immediately life-threatening, can serve as predisposing factors in facilitating the damage caused by suicidal behaviors or even contributing to other injuries that can be more dangerous than suicide itself. Therefore, clinical specialists should not only examine patients who attempt suicide to treat toxicity but also evaluate and provide care for other aspects that contribute to morbidity and mortality.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collecton and data interpretation: Saeed kargar-soleimanabad; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgments
The authors would like to express their special thanks to the patient for his consent to publishing his conditions as a case report.
Acute kidney injury (AKI), known as acute renal failure, refers to a sudden and irreversible decrease in overall kidney function over hours to days, resulting in the body’s inability to control electrolyte balance, water, acid, and base [1]. AKI is usually assessed by measuring glomerular filtration rate (GFR) and increased levels of creatinine, in addition to blood urea nitrogen and fractional sodium excretion in some cases. The exact prevalence of AKI in the general population is unknown; however, studies have shown a 7% prevalence in hospitalized patients and 30% in ICU patients, indicating that a large number of patients admitted to medical and ICU wards, as well as non-hospitalized patients are at risk for AKI [2]. This high prevalence reflects AKI as a serious challenge for healthcare systems. An increase in complications usually accompanies the occurrence of AKI, the possibility of progression to chronic kidney disease (CKD), as well as short-term and long-term mortality. Patients requiring dialysis and renal replacement therapy have about 50 times higher chances of progressing toward chronic kidney diseases [3].
AKI is a complex clinical syndrome classified into the following three categories based on the anatomical site of involvement: Prerenal, intrinsic renal, and postrenal. AKI with intrinsic origin is classified based on the site of involvement in the kidney, which includes tubules, glomeruli, renal vessels, and interstitial tissue. Causes of intrinsic injury include prolonged hypo-perfusion, sepsis, and nephrotoxins. These toxins can originate from within the body, such as hemoglobin and myoglobin, or from outside the body, such as drugs like aminoglycosides, vancomycin, amphotericin, and pentamidine [4].
Rhabdomyolysis is a clinical event characterized by muscle damage, disruption of muscle fibers, and release of intracellular contents into the bloodstream. Myoglobin, creatine phosphokinase, and lactate dehydrogenase are among the main intracellular contents of muscle that are used to assess the extent of damage [5]. The most common clinical manifestations of rhabdomyolysis are myalgia, fatigue, red-colored urine, and swelling in the affected muscle; however, it can also present with less common and nonspecific symptoms, such as fever, nausea, vomiting, and dyspnea. The leading causes of rhabdomyolysis include trauma, drugs such as statins, toxins, temperature extremes, excessive physical activity, and inherited and acquired metabolic disorders in the muscle [6].
Case Presentation
A 40-year-old male patient was transferred to the emergency department by EMS with complaints of decreased consciousness. The patient reported ingesting 40 tablets of 20 mg methadone, 27 tablets of 10 mg nortriptyline, and 13 tablets of 2 mg clonazepam three days before admission. He had been in his room for the past three days and had not eaten or urinated. In terms of medical history, the patient had a history of addiction and had been on daily methadone treatment for 20 days, which he stopped two months ago. He also mentioned several unsuccessful suicide attempts with methadone. His past psychiatry history included major depression disorder and substance abuse for more than ten years.
On initial examination, the patient weighed approximately 70 kg, had a blood pressure of 85/60, a heart rate of 70 beats per minute, a respiratory rate of 15 breaths per minute, and a Glasgow coma scale score of 10. The patient had extensive erythema on the right side of his body, which was caused by prolonged lying on that side. The erythema involved the right arm, right side of the body, and right leg. The patient confirmed that he had been lying in this position for two days without changing. There were also blisters on the posterior aspect of the shoulder joint, the forearm, and the right side of the patient’s body. Due to decreased consciousness and drowsiness, the patient could not express his main complaint; however, weakness and muscle pain, especially on the right side of the body, were apparent on physical examination.
Complete laboratory tests, electrocardiogram, and toxicology consult were requested for the patient; laboratory tests showed respiratory acidosis partially compensated by metabolic alkalosis. The patient had increased creatinine levels, liver enzymes (aspartate transaminase approximately 14 times normal, alanine transaminase approximately six times normal), and creatine phosphokinase-MB (approximately 230 times normal; Table 1).
Based on the clinical symptoms, AKI following rhabdomyolysis was suspected in the patient, which was confirmed by laboratory results. As the first step, intravenous hydration was initiated for the patient, and fluid intake and output were monitored. Kidney function tests, electrolytes, and daily consultations with toxicology were requested for the patient. One day after treatment, the respiratory acidosis was corrected, and on the fourth day of hospitalization, the patient’s creatinine level returned to 1.2 mg/dL, which was in the normal range. The patient was discharged with a good general condition.
Discussion
Some commentators define the term “suicidal behaviors” as a general term that encompasses all thoughts and actions related to suicide without distinguishing between thoughts and plans, non-lethal acts, and acts that result in death. Suicide is now recognized as one of the leading causes of death, morbidity, and disability worldwide. The level of effort and success in suicide attempts varies depending on different circumstances; however, epidemiological studies have shown that age, gender, socioeconomic status, geographical location, and country of residence have an impact on the rate of suicide attempts and their success [7]. Among these factors, the rate of suicide attempts is higher in older individuals, and mortality rates are higher in males, with suicide attempts in women being twice as high as in men. However, the methods used by women are less lethal, and the mortality and success rates in completing suicide are higher in older individuals. Different individuals choose different suicide methods based on their circumstances and preferences. However, methods such as hanging, using firearms, suffocation, jumping from heights, and drug poisoning are the most common and widely used methods of suicide [8]. The simultaneous use of multiple methods for suicide is referred to as “complex suicide.” In some cases of complex suicide, an individual may use multiple drugs, and the simultaneous use of multiple drugs with different pharmacokinetics and pharmacodynamics can affect the course of the disease and the effectiveness of therapeutic interventions [9]. Suicide attempts are often carried out using drugs, with benzodiazepines, antipsychotics, barbiturates, and antidepressants having the highest rates of use. According to many studies, benzodiazepines are used for suicide along with other drugs that have suppressive effects on the nervous system [10]. In the present case study, a 40-year-old male patient with a previous history of suicide attempts presented to the emergency department after ingesting methadone, clonazepam, and nortriptyline.
Methadone is a fully synthetic opioid with a long duration of action that is similar to morphine but does not have the same potency. Similar to other opioids, this drug binds to opioid receptors on the surface of cells in the central nervous system, lungs, heart, blood vessels, and intestines and has a similar mechanism of action. Therefore, the high dosage of this drug can cause symptoms of central nervous system and respiratory suppression, leading to decreased consciousness, sedation, and bradypnea. On the other hand, the patient in this study had consumed a significant amount of clonazepam, which, when used concurrently with opioids, can exacerbate respiratory and nervous system suppression [11]. Predictably, without antidote use, the patient would experience decreased levels of consciousness and sedation for approximately 48 h. Additionally, the patient had consumed an excessive amount of nortriptyline, which can also cause reduced consciousness, muscle involvement, and muscle stiffness as symptoms of toxicity. Considering this drug overdose in a complex manner in this patient, it was expected that he would experience decreased levels of consciousness and sedation for approximately 48 h. Furthermore, due to the patient’s companions not paying attention to his prolonged sleep, lack of movement, and failure to change position during the intoxication period, rhabdomyolysis was suspected based on the patient’s clinical symptoms, including extensive erythema on the right side and pain on palpation [12]. Laboratory results confirmed this diagnosis. Considering that rhabdomyolysis and the release of intracellular contents such as myoglobin can cause damage to kidney tissue and lead to AKI. A workup for AKI was performed for the patient. With early treatment initiation, the extent of kidney damage did not progress, and the patient’s creatinine level did not exceed 1.6, resulting in a stable condition.
Although direct drug poisoning did not cause death or organ damage in this case, the decrease in consciousness level, which is one of the main adverse effects of benzodiazepine and opioid poisoning, can create favorable conditions for events such as rhabdomyolysis, aspiration pneumonia, etc. leading to irreversible complications. In some cases, these complications may be more harmful than the risks associated with suicidal behaviors themselves.
Conclusion
The toxic effects lead to the creation of conditions that, although not immediately life-threatening, can serve as predisposing factors in facilitating the damage caused by suicidal behaviors or even contributing to other injuries that can be more dangerous than suicide itself. Therefore, clinical specialists should not only examine patients who attempt suicide to treat toxicity but also evaluate and provide care for other aspects that contribute to morbidity and mortality.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collecton and data interpretation: Saeed kargar-soleimanabad; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgments
The authors would like to express their special thanks to the patient for his consent to publishing his conditions as a case report.
References
- Kellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders HJ. Acute kidney injury. Nat Rev Dis Primers. 2021; 7(1):52. [DOI:10.1038/s41572-021-00284-z] [PMID]
- Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019; 394(10212):1949-64. [DOI:10.1016/S0140-6736(19)32563-2] [PMID]
- Levey AS, James MT. Acute kidney injury. Ann Intern Med. 2017; 167(9):ITC66-80. [DOI:10.7326/AITC201711070] [PMID]
- Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009; 361(1):62-72. [DOI:10.1056/NEJMra0801327] [PMID]
- Cabral BMI, Edding SN, Portocarrero JP, Lerma EV. Rhabdomyolysis. Dis Mon. 2020; 66(8):101015. [DOI:10.1016/j.disamonth.2020.101015] [PMID]
- Baeza-Trinidad R. Rhabdomyolysis: A syndrome to be considered. Med Clin (Barc). 2022; 158(6):277-83. [DOI:10.1016/j.medcli.2021.09.025] [PMID]
- Hawton K, van Heeringen K. Suicide. Lancet. 2009; 373(9672):1372-81. [DOI:10.1016/S0140-6736(09)60372-X]
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies: A systematic review. JAMA. 2005; 294(16):2064-74. [DOI:10.1001/jama.294.16.2064] [PMID]
- Hawton K, Van Heeringen K. The international handbook of suicide and attempted suicide. New Jersey: John Wiley & Sons; 2000. [DOI:10.1002/9780470698976]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008; 192(2):98-105. [DOI:10.1192/bjp.bp.107.040113] [PMID]
- Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: A continuing tragedy in developing countries. Int J Epidemiol. 2003; 32(6):902-9. [DOI:10.1093/ije/dyg307] [PMID]
- Sher L. Alcohol consumption and suicide. QJM. 2006; 99(1):57-61. [DOI:10.1093/qjmed/hci146] [PMID]
Type of Study: case report |
Subject:
Drug Clinical Investigation
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |