Volume 9, Issue 1 (2023)
Pharm Biomed Res 2023, 9(1): 73-76 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseini S H, Zamani N, Ahmadi A. Fluoxetine-induced Hypotension: A Case Report. Pharm Biomed Res 2023; 9 (1) :73-76
URL: http://pbr.mazums.ac.ir/article-1-362-en.html
URL: http://pbr.mazums.ac.ir/article-1-362-en.html
1- Psychiatry and Behavioral Sciences Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran.
2- Student Research Committee, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari, Iran.
3- Pharmaceutical Sciences Research Center, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari, Iran.
2- Student Research Committee, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari, Iran.
3- Pharmaceutical Sciences Research Center, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 484 kb]
(1260 Downloads)
| Abstract (HTML) (3016 Views)
Full-Text: (12380 Views)
1. Introduction
Blood pressure is regulated via the autonomic nervous system. The sympathetic nervous system acts to raise blood pressure, and the parasympathetic nervous system lowers blood pressure [1]. Hypotension is a decrease in systemic blood pressure (less than 90/60 mmHg). Although often harmless, this can also be dangerous [2]. It is under-recognized, mainly because it has few or even no symptoms. Symptoms occur as a result of hypoperfusion of essential organs [3]. According to the criteria of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), Mixed Anxiety and Depression Disorder (MADD) is characterized by subsyndromal symptoms of anxiety and depression (i.e., symptoms that are severe enough to justify the diagnosis of MADD, but none of them are predominant enough to insure a separate diagnosis of an underlying anxiety disorder or depression) [4]. MADD may occur at any age [5], and patients often present with severe physical, social, and psychological impairment. Symptoms are more disabling and resistant to treatment than those of either condition (anxiety or depression) alone [6].
Fluoxetine is an Selective Serotonin Reuptake Inhibitors (SSRIs) that exerts its anti-depressive effect by blocking the presynaptic reuptake of the neurotransmitter serotonin, 5-hydroxytryptophan (5-HT). The high affinity of fluoxetine for 5-HT transporters, minimal activity on noradrenergic reuptake, and no affinity for dopamine transporters indicate that it is 5-HT-selective [7, 8]. Most side effects of SSRIs are dose-dependent, time-dependent, and can be attributed to serotonergic effects. Serotonin receptors mediate a variety of functions, including sleep, appetite, and sexual functions. Sleep disturbance, weight gain, and sexual dysfunction are the most bothering adverse effects during long-term SSRI therapy. In general, the most common side effects of the medication include insomnia, nausea, diarrhea, anorexia, yawning, headache, libido loss, weakness, tremor, and pharyngitis [9, 10, 11]. To the best of our knowledge, hypotension induced by fluoxetine has been not reported in any international literature. Herein, we report the first case of hypotension caused by fluoxetine in a young woman with MADD.
2. Case Report
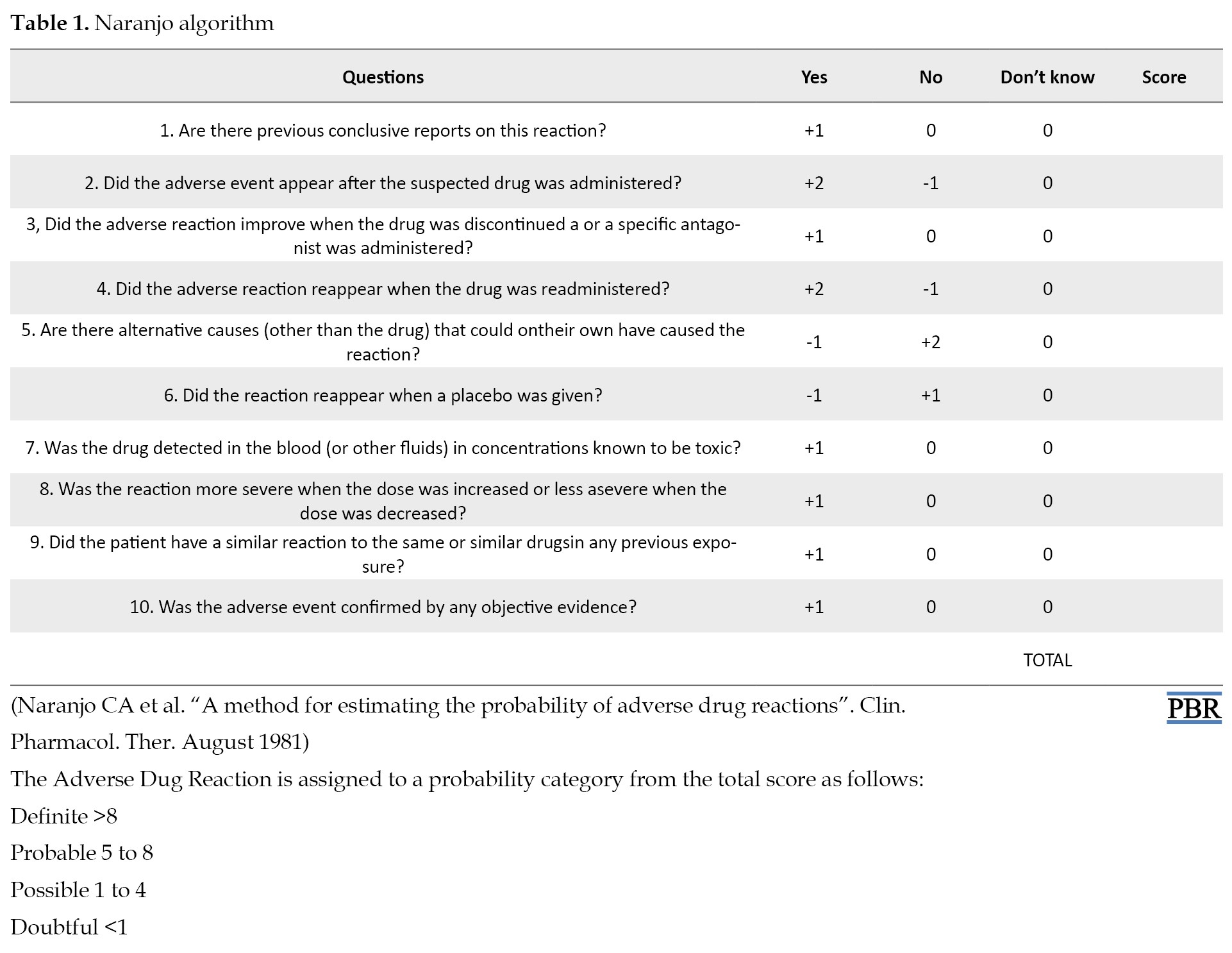
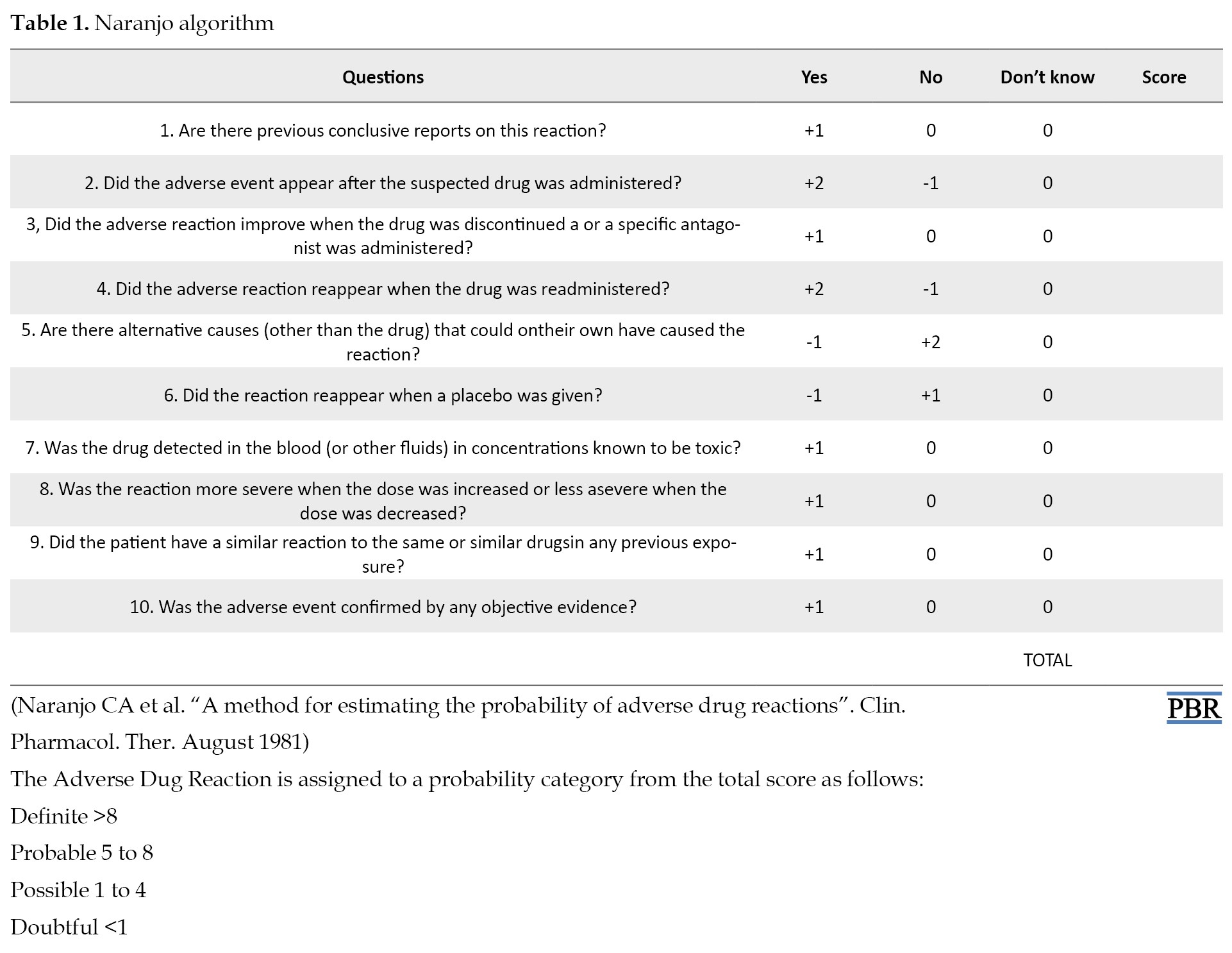
A 35-year-old female attended our clinic with symptoms of depression, anxiety, lack of enjoyment of life, intolerance, thoughts of despair, weakness, fatigue, and insomnia. After the initial mental status examination, she was diagnosed with a case of MADD, and treatment was initiated under our care service with 10 mg/day fluoxetine and 0.5 mg/day alprazolam. After one week, the daily fluoxetine dosage was increased to 20 mg. After increasing the drug dose, the patient complained of dizziness, lethargy, and a feeling of weakness in the lower limbs. She was brought to our emergency service with a blood pressure of 80/60 mmHg. Before starting fluoxetine, the patient’s blood pressure was 110/70 mmHg and she had no history of physical illness, fainting, or hypotension. She also had a negative family history of hypotension. Complete laboratory examinations, including complete blood count, serum electrolytes, liver function test, renal function test, thyroid function test, and urine analysis were done and all reports were within normal limits. Some probable clinical conditions that can cause hypotension, such as dehydration, anemia, malnutrition, hyponatremia, congestive heart failure, arrhythmia, atrial fibrillation, vascular disease, and use of other medications were excluded. Her chest X-ray and electrocardiography results were found to be normal and provided no explanation for hypotension. The patient’s hypotension could not be due to orthostatic hypotension. While blood pressure was measured while sitting and standing, no change was observed and the patient’s symptoms did not worsen during the standing position. Although fluoxetine is usually associated with hypertension, we hypothesized that the patient’s hypotension might be caused by fluoxetine. Thus, the patient was asked to stop taking fluoxetine. After discontinuing the use of fluoxetine, the hypotension symptoms disappeared. One month later, the patient resumed fluoxetine again and was told to stop taking it and return to the clinic immediately if the recurrence of the previously described symptoms occurred. Six days after resuming the drug, she presented with similar symptoms and blood pressure of 85/60 mmHg. Finally, another SSRI agent was replaced with fluoxetine, and alprazolam was continued at 0.5 mg/day. The rapid disappearance of hypotension after discontinuation of fluoxetine, indicates a relationship between the mentioned effect and the drug. Consequently, according to the Naranjo causality scale (which showed a score of 8), this adverse effect was probably induced by fluoxetine. Thus, fluoxetine was replaced by another SSRI agent and alprazolam continued with the previous dose. After she discontinued fluoxetine, hypotension did not occur again (Table 1).
3. Discussion
Fluoxetine is usually considered safe for most patients. To the best of our knowledge, this is the first case report that correlates a regular fluoxetine dose with the presence of hypotension. A two-factor convergence can demonstrate the association between hypotension and fluoxetine: manifesting hypotension while prescribing an increasing dose of fluoxetine and improving hypotension by discontinuing the medication. These factors provide a dose-dependent relationship between a decrease in blood pressure and taking fluoxetine. Antidepressant drugs are often associated with cardiovascular side effects and toxicity, such as hypertension, prolonged PR (the PR interval is the time from the beginning of the P wave (arterial depolarization) to the beginning of the QRS complex (ventricular depolarization)), arrhythmia, and hypotension [12, 13, 14, 15]. Various clinical studies on SSRIs, such as fluoxetine, citalopram, and sertraline, have indicated remarkable advantages over Tricyclic Antidepressants (TCAs) because of causing fewer cardiotoxic side effects during the treatment of depressive disorders. These newer compounds have demonstrated a lower risk of inducing hypotension [13]; however, an increasing number of case reports have indicated that the use of SSRIs is associated with cases of orthostatic hypotension in patients without cardiovascular disorders [16]. Orthostatic hypotension is defined as a decrease in systolic blood pressure of at least 20 mmHg or a decrease in diastolic blood pressure of at least 10 mmHg within three minutes upon standing from sitting or from a lying position. Since orthostatic hypotension can be a side effect of many antidepressants, we decided to measure the patient’s blood pressure in different situations for further investigation. After comparing systolic and diastolic blood pressure in different positions, it was found that the patient’s hypotension was not orthostatic [17]. In a study carried out by Fuller et al., an antihypertensive effect of the combination of fluoxetine and 5-HTP in Deoxycorticosterone acetate (DOCA)-salt hypertensive rats was demonstrated. Fluoxetine alone had also a remarkable antihypertensive effect on blood pressure. As it is suggested that boosting central serotonergic function lowers blood pressure, they hypothesized that the mechanism of lowering blood pressure by fluoxetine and 5-HTP (as a chemical precursor of serotonin) might be related to the enhancement of the central serotonin function and diminished central sympathetic neural outflow [18]. A significant lowering effect of venlafaxine (as a serotonin and noradrenaline reuptake inhibitor) on blood pressure was reported in a female patient with a history of Major Depressive Disorder (MDD). Participation of presynaptic α2-adrenergic receptors was considered to be a pathophysiological mechanism to describe the relationship between taking a regular dose of venlafaxine and the development of symptomatic hypotension [19]. Therefore, the occurrence of hypotension cannot be attributed to the case reported in our case report as fluoxetine has little or no affinity for α2-adrenergic receptors. Since fluoxetine does not have a direct cardiac or vascular effect, the reduction of blood pressure may be due to a central action of fluoxetine on the vasomotor center [16].
Here, this is the first report on the development of hypotension following the use of a regular dose of fluoxetine. Although further studies are needed to clarify this side effect, it may be important for the physicians to be aware of this rare situation and recommend discontinuing the drug immediately if complications have occurred.
Ethical Considerations
Compliance with ethical guidelines
All related research's ethical principles are considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Visited and followed up the patient and gathered the data: Hamzeh Hosseini; Analyzed the data and wrote the article: Neda Zamani; Critically revised the final draft of the manuscript: Amirhossein Ahmadi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Hosseini for providing information about the studied patients.
References
Blood pressure is regulated via the autonomic nervous system. The sympathetic nervous system acts to raise blood pressure, and the parasympathetic nervous system lowers blood pressure [1]. Hypotension is a decrease in systemic blood pressure (less than 90/60 mmHg). Although often harmless, this can also be dangerous [2]. It is under-recognized, mainly because it has few or even no symptoms. Symptoms occur as a result of hypoperfusion of essential organs [3]. According to the criteria of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), Mixed Anxiety and Depression Disorder (MADD) is characterized by subsyndromal symptoms of anxiety and depression (i.e., symptoms that are severe enough to justify the diagnosis of MADD, but none of them are predominant enough to insure a separate diagnosis of an underlying anxiety disorder or depression) [4]. MADD may occur at any age [5], and patients often present with severe physical, social, and psychological impairment. Symptoms are more disabling and resistant to treatment than those of either condition (anxiety or depression) alone [6].
Fluoxetine is an Selective Serotonin Reuptake Inhibitors (SSRIs) that exerts its anti-depressive effect by blocking the presynaptic reuptake of the neurotransmitter serotonin, 5-hydroxytryptophan (5-HT). The high affinity of fluoxetine for 5-HT transporters, minimal activity on noradrenergic reuptake, and no affinity for dopamine transporters indicate that it is 5-HT-selective [7, 8]. Most side effects of SSRIs are dose-dependent, time-dependent, and can be attributed to serotonergic effects. Serotonin receptors mediate a variety of functions, including sleep, appetite, and sexual functions. Sleep disturbance, weight gain, and sexual dysfunction are the most bothering adverse effects during long-term SSRI therapy. In general, the most common side effects of the medication include insomnia, nausea, diarrhea, anorexia, yawning, headache, libido loss, weakness, tremor, and pharyngitis [9, 10, 11]. To the best of our knowledge, hypotension induced by fluoxetine has been not reported in any international literature. Herein, we report the first case of hypotension caused by fluoxetine in a young woman with MADD.
2. Case Report
A 35-year-old female attended our clinic with symptoms of depression, anxiety, lack of enjoyment of life, intolerance, thoughts of despair, weakness, fatigue, and insomnia. After the initial mental status examination, she was diagnosed with a case of MADD, and treatment was initiated under our care service with 10 mg/day fluoxetine and 0.5 mg/day alprazolam. After one week, the daily fluoxetine dosage was increased to 20 mg. After increasing the drug dose, the patient complained of dizziness, lethargy, and a feeling of weakness in the lower limbs. She was brought to our emergency service with a blood pressure of 80/60 mmHg. Before starting fluoxetine, the patient’s blood pressure was 110/70 mmHg and she had no history of physical illness, fainting, or hypotension. She also had a negative family history of hypotension. Complete laboratory examinations, including complete blood count, serum electrolytes, liver function test, renal function test, thyroid function test, and urine analysis were done and all reports were within normal limits. Some probable clinical conditions that can cause hypotension, such as dehydration, anemia, malnutrition, hyponatremia, congestive heart failure, arrhythmia, atrial fibrillation, vascular disease, and use of other medications were excluded. Her chest X-ray and electrocardiography results were found to be normal and provided no explanation for hypotension. The patient’s hypotension could not be due to orthostatic hypotension. While blood pressure was measured while sitting and standing, no change was observed and the patient’s symptoms did not worsen during the standing position. Although fluoxetine is usually associated with hypertension, we hypothesized that the patient’s hypotension might be caused by fluoxetine. Thus, the patient was asked to stop taking fluoxetine. After discontinuing the use of fluoxetine, the hypotension symptoms disappeared. One month later, the patient resumed fluoxetine again and was told to stop taking it and return to the clinic immediately if the recurrence of the previously described symptoms occurred. Six days after resuming the drug, she presented with similar symptoms and blood pressure of 85/60 mmHg. Finally, another SSRI agent was replaced with fluoxetine, and alprazolam was continued at 0.5 mg/day. The rapid disappearance of hypotension after discontinuation of fluoxetine, indicates a relationship between the mentioned effect and the drug. Consequently, according to the Naranjo causality scale (which showed a score of 8), this adverse effect was probably induced by fluoxetine. Thus, fluoxetine was replaced by another SSRI agent and alprazolam continued with the previous dose. After she discontinued fluoxetine, hypotension did not occur again (Table 1).
3. Discussion
Fluoxetine is usually considered safe for most patients. To the best of our knowledge, this is the first case report that correlates a regular fluoxetine dose with the presence of hypotension. A two-factor convergence can demonstrate the association between hypotension and fluoxetine: manifesting hypotension while prescribing an increasing dose of fluoxetine and improving hypotension by discontinuing the medication. These factors provide a dose-dependent relationship between a decrease in blood pressure and taking fluoxetine. Antidepressant drugs are often associated with cardiovascular side effects and toxicity, such as hypertension, prolonged PR (the PR interval is the time from the beginning of the P wave (arterial depolarization) to the beginning of the QRS complex (ventricular depolarization)), arrhythmia, and hypotension [12, 13, 14, 15]. Various clinical studies on SSRIs, such as fluoxetine, citalopram, and sertraline, have indicated remarkable advantages over Tricyclic Antidepressants (TCAs) because of causing fewer cardiotoxic side effects during the treatment of depressive disorders. These newer compounds have demonstrated a lower risk of inducing hypotension [13]; however, an increasing number of case reports have indicated that the use of SSRIs is associated with cases of orthostatic hypotension in patients without cardiovascular disorders [16]. Orthostatic hypotension is defined as a decrease in systolic blood pressure of at least 20 mmHg or a decrease in diastolic blood pressure of at least 10 mmHg within three minutes upon standing from sitting or from a lying position. Since orthostatic hypotension can be a side effect of many antidepressants, we decided to measure the patient’s blood pressure in different situations for further investigation. After comparing systolic and diastolic blood pressure in different positions, it was found that the patient’s hypotension was not orthostatic [17]. In a study carried out by Fuller et al., an antihypertensive effect of the combination of fluoxetine and 5-HTP in Deoxycorticosterone acetate (DOCA)-salt hypertensive rats was demonstrated. Fluoxetine alone had also a remarkable antihypertensive effect on blood pressure. As it is suggested that boosting central serotonergic function lowers blood pressure, they hypothesized that the mechanism of lowering blood pressure by fluoxetine and 5-HTP (as a chemical precursor of serotonin) might be related to the enhancement of the central serotonin function and diminished central sympathetic neural outflow [18]. A significant lowering effect of venlafaxine (as a serotonin and noradrenaline reuptake inhibitor) on blood pressure was reported in a female patient with a history of Major Depressive Disorder (MDD). Participation of presynaptic α2-adrenergic receptors was considered to be a pathophysiological mechanism to describe the relationship between taking a regular dose of venlafaxine and the development of symptomatic hypotension [19]. Therefore, the occurrence of hypotension cannot be attributed to the case reported in our case report as fluoxetine has little or no affinity for α2-adrenergic receptors. Since fluoxetine does not have a direct cardiac or vascular effect, the reduction of blood pressure may be due to a central action of fluoxetine on the vasomotor center [16].
Here, this is the first report on the development of hypotension following the use of a regular dose of fluoxetine. Although further studies are needed to clarify this side effect, it may be important for the physicians to be aware of this rare situation and recommend discontinuing the drug immediately if complications have occurred.
Ethical Considerations
Compliance with ethical guidelines
All related research's ethical principles are considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Visited and followed up the patient and gathered the data: Hamzeh Hosseini; Analyzed the data and wrote the article: Neda Zamani; Critically revised the final draft of the manuscript: Amirhossein Ahmadi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank Hosseini for providing information about the studied patients.
References
- Althunayyan SM. Shock index as a predictor of post-intubation hypotension and cardiac arrest; a review of the current evidence. Bull Emerg Trauma. 2019; 7(1):21-7. [PMID] [PMCID]
- Cheshire WP. Chemical pharmacotherapy for the treatment of orthostatic hypotension. Expert Opin Pharmacother. 2019; 20(2):187-99. [PMID]
- Bonanno FG. Clinical pathology of the shock syndromes. J Emerg Trauma Shock. 2011; 4(2):233-43. [DOI:10.4103/0974-2700.82211] [PMID] [PMCID]
- World Health Organization. International statistical classification of diseases and related health problems: Tenth revision, 2nd ed. Geneva: World Health Organization; 2004. https://apps.who.int/iris/handle/10665/42980
- Angst J, Merikangas K. The depressive spectrum: Diagnostic classification and course. J Affect Disord. 1997; 45(1-2):31-40. [DOI:10.1016/S0165-0327(97)00057-8]
- Tiller JW, Franzcp F. Depression and anxiety. Med J Aust. 2013; 199(S6):S28-31. [DOI:10.5694/mja12.10628]
- Robertson OD, Coronado NG, Sethi R, Berk M, Dodd S. Putative neuroprotective pharmacotherapies to target the staged progression of mental illness. Early Interv Psychiatry. 2019; 13(5):1032-49. [DOI:10.1111/eip.12775] [PMID]
- Cao B, Zhu J, Zuckerman H, Rosenblat JD, Brietzke E, Pan Z, et al. Pharmacological interventions targeting anhedonia in patients with major depressive disorder: A systematic review. Prog Neuropsychopharmacol Biol Psychiatry. 2019; 92:109-17. [DOI:10.1016/j.pnpbp.2019.01.002] [PMID]
- Ferguson JM. SSRI antidepressant medications: Adverse effects and tolerability. Prim Care Companion J Clin Psychiatry. 2001; 3(1):22-7. [PMID] [PMCID]
- Mullen S. Major depressive disorder in children and adolescents. Ment Health Clin. 2018; 8(6):275-83. [PMID] [PMCID]
- Bahar MA, Kamp J, Borgsteede SD, Hak E, Wilffert B. The impact of CYP2D6 mediated drug-drug interaction: A systematic review on a combination of metoprolol and paroxetine/fluoxetine. Br J Clin Pharmacol. 2018; 84(12):2704-15. [PMID] [PMCID]
- Glassman AH. Cardiovascular effects of tricyclic antidepressants. Annu Rev Med. 1984; 35:503-11. [DOI:10.1146/annurev.me.35.020184.002443] [PMID]
- Pacher P, Ungvari Z, Nanasi PP, Furst S, Kecskemeti V. Speculations on difference between tricyclic and selective serotonin reuptake inhibitor antidepressants on their cardiac effects. Is there any? Curr Med Chem. 1999; 6(6):469-80. [PMID]
- Burckhardt D, Raeder E, Müller V, Imhof P, Neubauer H. Cardiovascular effects of tricyclic and tetracyclic antidepressants. JAMA. 1978; 239(3):213-6. [PMID]
- Glassman AH, Bigger JT Jr. Cardiovascular effects of therapeutic doses of tricyclic antidepressants. A review. Arch Gen Psychiatry. 1981; 38(7):815-20. [PMID]
- Pacher P, Kecskemeti V. Cardiovascular side effects of new antidepressants and antipsychotics: new drugs, old concerns? Curr Pharm Des. 2004; 10(20):2463-75. [PMID] [PMCID]
- Chikkaramanjegowda V, de Leon J. Venlafaxine-induced orthostatic hypotension in a geriatric patient. Case Rep Psychiatry. 2013; 2013:761567. [PMID] [PMCID]
- Fuller RW, Holland DR, Yen TT, Bemis KG, Stamm NB. Antihypertensive effects of fluoxetine and L-5-hydroxytryptophan in rats.Life Sci. 1979; 25(14):1237-42. [PMID]
- Alexandrino-Silva C, Nadalini Mauá FH, de Andrade AG, de Toledo Ferraz Alves TC. Hypotension caused by therapeutic doses of venlafaxine: case report and proposed pathophysiological mechanisms. J Psychopharmacol. 2008; 22(2):214-6. [PMID]
Type of Study: case report |
Subject:
Clinical Pharmacy
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |










