Volume 7, Issue 1 (2021)
Pharm Biomed Res 2021, 7(1): 5-14 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Joda A, Ajetunmobi O, Olugbake O. Poisoning and its Management in Healthcare Facilities in Lagos State, Nigeria. Pharm Biomed Res 2021; 7 (1) :5-14
URL: http://pbr.mazums.ac.ir/article-1-330-en.html
URL: http://pbr.mazums.ac.ir/article-1-330-en.html
1- Department of Clinical Pharmacy and Biopharmacy, Faculty of Pharmacy, University of Lagos, Lagos, Nigeria.
Keywords: Poisoning, Healthcare provider, Antidotes, Poison control and management, Healthcare facilities
Full-Text [PDF 1184 kb]
(1991 Downloads)
| Abstract (HTML) (3298 Views)
Full-Text: (2335 Views)
Introduction
Poisoning is an important public health problem globally, and especially in children and teenagers [1, 2]. Every year, about 0.3 million people die from poisoning [3]. In 2012, WHO stated that an estimated number of 193460 people died worldwide from unintentional poisoning with 84% of these deaths occurring in low- and middle-income countries [1]. Another report in 2016 documented a mortality rate of 1.4 persons per 100000 population globally and 2.7 persons per 100000 population in Africa from unintentional poisoning [4]. Also, in 2012, it was documented that unintentional poisoning caused the loss of over 10.7 million years of healthy life (disability-adjusted life years, DALYs) [1].
Poisons are defined as chemical substances that produce harmful effects on entering the body. Poisoning may be natural, accidental, or deliberate (food sabotage, suicide terrorism) [2, 5, 6]. Most poisoning which occurs in children is accidental while intentional or suicidal poisoning occurs more in adolescents and adults where one purposely ingests a chemical to induce self-harm [2, 6].
WHO requires that its member states set up poison centers that advise on, and assists with the prevention, diagnosis, and management of poisoning. Currently, only 47% of the developed member states have one. As a result, healthcare providers are the main sources of help in the management of poisoning [7, 8]. In Nigeria, community pharmacists are the usual first port of call for many acute conditions while emergency units of general hospitals are for referral [9, 10]. There is a dearth of literature on the knowledge of healthcare providers about poisons and their antidotes and the modes and management of poisoning in general in Nigeria. This study set out to document the modes and management of poisoning cases and knowledge of specific antidotes by healthcare providers in selected community pharmacies and hospitals in Lagos state.
Materials and Methods
Study location and population
The study was carried out in Lagos State, Nigeria which has the highest population and largest number of healthcare providers among the other states of the federation [11]. Lagos is the largest cosmopolitan city in Nigeria that accommodates people of different tribes and cultures [12]. It is the largest cosmopolitan city in Nigeria with a rich and diverse culture of many tribes of different states. The study was conducted in two Local Government Areas (LGA) in Lagos State (Ikeja and Surulere LGA) among community pharmacists in registered pharmacies and emergency unit physicians in the secondary and tertiary hospitals. These local governments were chosen based on the location of the two teaching hospitals in the State: the Lagos University Teaching Hospital at Idiaraba, Surulere LGA, and the Lagos State University Teaching Hospital at Ikeja LGA.
Study design
The study was a multicentre, descriptive cross-sectional study among community pharmacists and emergency unit physicians. It was carried out to determine the knowledge and practices of selected healthcare providers about poisoning and its management as a baseline for future studies in this field.
Sampling
Forty community pharmacies were conveniently sampled from each LGA giving a total of 80 pharmacists recruited for the survey. Forty community pharmacies were conveniently selected per area from the list obtained from the Association of Community Pharmacists of Nigeria list for the areas. One pharmacist was chosen per pharmacy. In each LGA, the tertiary hospital and one secondary facility were selected for the survey. Six physicians from each secondary hospital and 10 from each tertiary hospital were chosen to give a total of 32 physicians. In total, 112 pharmacists and physicians (80 pharmacists and 32 physicians) were required for the survey.
Data collection tool
A pre-tested, semi-structured questionnaire was designed to collect relevant data for the study. The questionnaire had four sections: sociodemographic data; respondents’ knowledge and practice, follow-up activities, and poison control activities.
Data collection and analysis
The questionnaire was self-administered. Community pharmacists were approached in their pharmacies and informed consent was obtained before questionnaire administration. At the hospitals, physicians on duty at the emergency unit were approached and informed consent was obtained over two weeks. Respondents that were unable to complete it immediately after administration were given 2 weeks to fill it, after which another 2 weeks was given to mop up any remaining forms. The data obtained were collated and analyzed descriptively as frequencies (percentages), median, and mean as necessary. Inferential statistics were determined using the Student t test. All analyses were carried out with the SPSS version 20.0. P<0.05 were considered statistically significant. Results were presented as frequency tables and charts.
Study outcomes
The outcomes for this study were to document the modes of poisoning cases encountered by the healthcare providers and the usual management of poisoning cases, and finally to determine the knowledge of specific antidotes by healthcare providers. A comparison of the knowledge between the two provider groups studied was also determined. Finally, respondents’ perception of poisoning management in their facilities, availability of poisoning management protocols, and challenges associated with poisoning were additional outcomes.
Results
A total of 96 responses were received, 65 community pharmacists and 31 physicians from the hospitals, giving a response rate of 85.7% (81.3% for the pharmacists and 96.9% for the physicians). All 96 obtained responses were filled and eligible for analysis. Most respondents were female (52.1%) and in the age range of 30-39 years (41.7%); over 83% had had no specialized training on poisoning management. The most common mode of poisoning encountered was accidental (89% and 68% among pharmacists and physicians, respectively) (Table 1).
.jpg)
Contaminated food, alcohol, and kerosene were the agents most commonly implicated in poisoning cases (Table 2).
.jpg)
The majority of the respondents saw less than one poisoning case per month (48.8%) and most of the cases were among children between 0 and 5 years old (41.5% and 48.3% among pharmacists and physicians, respectively). In almost all cases, some form of home remedy or the other had been tried by caregivers (Table 3).
.jpg)
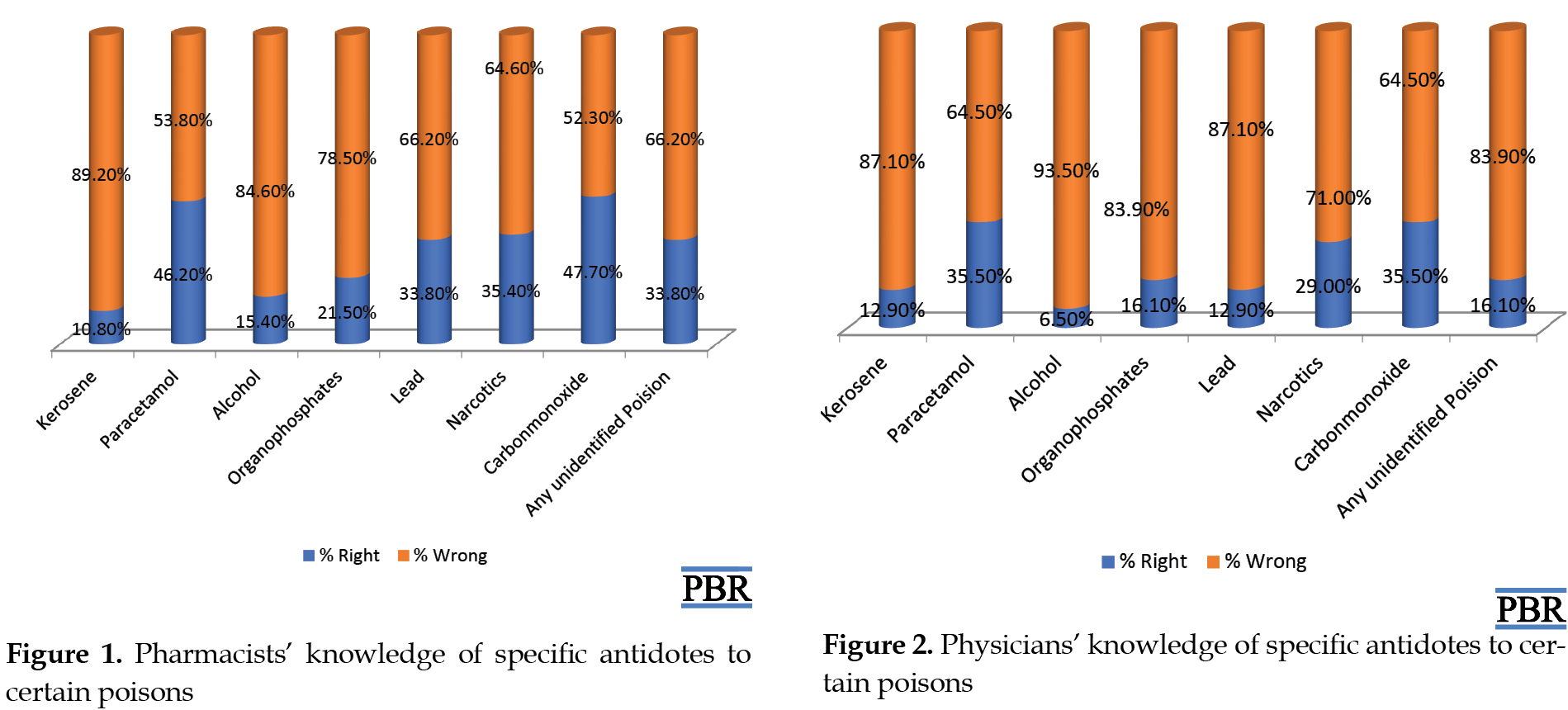
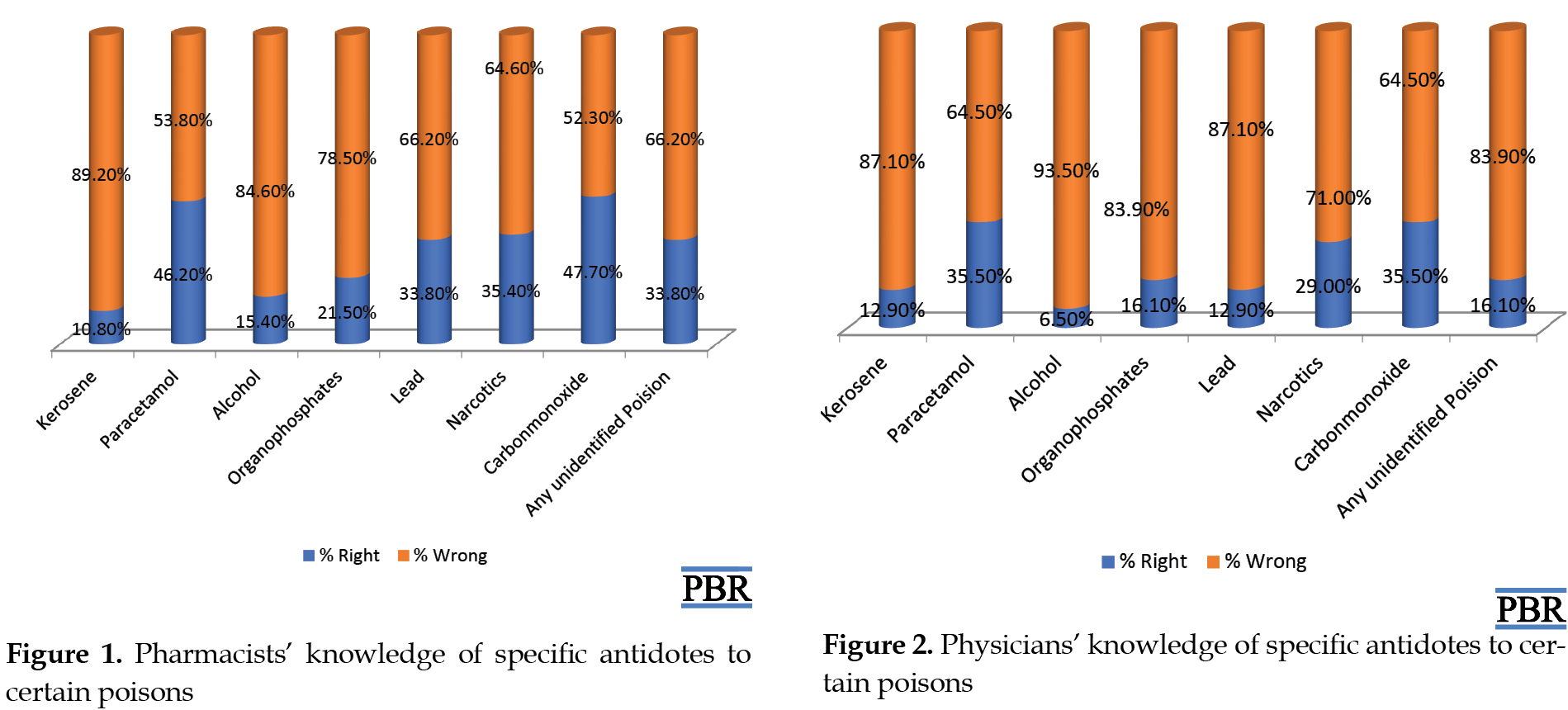
Most of the respondents had poor knowledge about the antidotes to use for different poisons they were presented with. The highest response rate was for antidotes for carbon monoxide and paracetamol (pharmacists at 48% and 46%, respectively; physicians 36% each). Though knowledge was generally poor, pharmacists had a higher mean score than the physicians and the difference in result was statistically significant (P=0.000) (Figures 1 and 2, Table 4).
.jpg)
Referral was the main strategy of management by the pharmacists (33%) while supportive care was the most common strategy utilized by the physicians (61%). Both groups commonly employed specific antidotes (about 42%) (Figure 3). Poisoning management protocols were not available at the facilities surveyed either in the form of guidelines or standard operating procedures/processes or specific antidotes. About 62% of the respondents indicated that poisoning management is inadequate in their facilities (Table 5). The healthcare providers indicated that lack of specific antidotes, required equipment and necessary knowledge were some challenges faced in providing adequate poisoning management (Figure 4). Discussion
This study describes the types and management of poisoning cases and knowledge of specific antidotes by healthcare providers. The study revealed that contaminated food, alcohol, and kerosene were the common agents implicated in poisoning. These agents were followed by household cleaning agents, drugs, and organophosphates. Contaminated food and kerosene may not be surprising as Nigeria has poor access to improved water and sanitation and kerosene is still a major source of fuel for cooking and other household use e.g., as a source of light and heat [13, 14]. These agents were similarly implicated in studies in Enugu, South-Eastern Nigeria, Tanzania, and East Africa [15, 16, 17]. However, studies from other parts of the world reveal that in general, drugs are more common sources of poisoning in the Western world and pesticides in many parts of Asia [18, 19]. The difference in the responses for contaminated food and kerosene were statistically significant between the two groups of respondents.
Demographic details show statistically significant differences in the age range of respondents and years in practice. Most of the respondents are below 40 years of age. The majority of the cases seen by the healthcare providers were accidental though the physicians saw more intentional cases. About half of the accidental cases were in children under 12 with the majority being under 5. Accidental poisoning in children remains a source of concern worldwide but most especially in developing countries [20, 21, 22]. This is a major gap that shows that the education of parents and caregivers in the handling and storage of food and other poisonous items have to be reinforced. The difference in the age group commonly affected by poisoning is statistically significant between the two groups.
There have been more intentional suicide cases among teenagers [23] and this study noted more intentional cases among teenagers similar to a study in Iran where most cases are seen were intentional and among teenagers and young adults (85%) [7, 23]. The difference in the forms of poisoning encountered by respondents is statistically significant.
There are a lot of myths about home-made remedies as antidotes to poisoning but there is a dearth of literature to confirm these claims. Both healthcare providers had heard about home remedies and found that the caregivers had used home management strategies of palm oil, milk, or eggs which are used to initiate vomiting or thought to neutralize the effects of the ingested poison.
Knowledge of antidotes by both pharmacists and physicians was poor even though knowledge gaps varied as shown in previous studies [24, 25]. The difference obtained in this result was statistically significant (P=0.000). This is a gap that needs to be rectified through the training of the various healthcare providers, especially since about four-fifths of the respondents said they had not received any training on poisoning.
The main method of management by the pharmacist was the use of antidotes, referrals, and first aid. Due to their accessibility and skills and services in medication management, they are the first port of call for medical assistance in the community [26]. Management by physicians was supportive of the use of antidotes. This is in line with literature in which supportive care should be the mainstay in poisoning management [27].
The availability of antidotes and poisoning management was generally poor in this study. The majority of the physicians were not aware of the availability of poisoning management protocols in their healthcare facilities, while just under a third of pharmacists said they had guidelines for the management of standard operating procedures. The difference in the availability of poisoning management protocol in the facility is statistically significant between the two groups of respondents. The main challenges faced were a lack of antidotes, adequate equipment, and knowledge. As expected, activated charcoal was largely available, especially in the community pharmacies. The unavailability of antidotes in healthcare facilities has been widely reported by other studies [25, 28, 29, 30].
The need for a poison control center was recognized by most respondents in this study with most feeling that poison cases should be reported to a central poison center. Other studies also recognized the importance of poison control centers [2, 31, 32, 33, 34]. A previous study showed that establishing poison information centers in different parts of the country, preparing national treatment guidelines, training healthcare providers, and ensuring the availability of, and easy access to antidotes were the issues that must be solved to ensure proper management of poisoning in healthcare facilities. Other proposed solutions include education on the importance of stocking antidotes, regular review of storage of antidotes, development of distribution plans, and the development of antidote guidelines. Future research to improve the management of poisoning was also recommended [25, 28, 29, 30, 31, 32, 33, 34].
The study was limited to two locations which were conveniently chosen and sampled healthcare providers hence the results may not be generalizable though it provides useful information for planning and further studies, especially among community pharmacists and physicians.
Knowledge of antidotes to various poisons was poor and management of poisoning was largely inadequate. The establishment of poison control centers in healthcare facilities and the organization of updated lectures and training for community pharmacists and physicians will go a long way to improving poisoning management in the state.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Lagos University Teaching Hospital (LUTH) Research and Ethics Committee. Approval to use facilities was obtained from the individual hospitals, as well as the Association of Community Pharmacists of Nigeria (ACPN), Lagos State Branch.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology: Arinola Joda, Oluwaseun Ajetunmobi; Investigation, writing – review & editing: All authors; Writing – original draft: Arinola Joda, Olubusola Olugbake.
Conflict of interest
The authors declare no conflict of interest associated with this study.
References
Poisoning is an important public health problem globally, and especially in children and teenagers [1, 2]. Every year, about 0.3 million people die from poisoning [3]. In 2012, WHO stated that an estimated number of 193460 people died worldwide from unintentional poisoning with 84% of these deaths occurring in low- and middle-income countries [1]. Another report in 2016 documented a mortality rate of 1.4 persons per 100000 population globally and 2.7 persons per 100000 population in Africa from unintentional poisoning [4]. Also, in 2012, it was documented that unintentional poisoning caused the loss of over 10.7 million years of healthy life (disability-adjusted life years, DALYs) [1].
Poisons are defined as chemical substances that produce harmful effects on entering the body. Poisoning may be natural, accidental, or deliberate (food sabotage, suicide terrorism) [2, 5, 6]. Most poisoning which occurs in children is accidental while intentional or suicidal poisoning occurs more in adolescents and adults where one purposely ingests a chemical to induce self-harm [2, 6].
WHO requires that its member states set up poison centers that advise on, and assists with the prevention, diagnosis, and management of poisoning. Currently, only 47% of the developed member states have one. As a result, healthcare providers are the main sources of help in the management of poisoning [7, 8]. In Nigeria, community pharmacists are the usual first port of call for many acute conditions while emergency units of general hospitals are for referral [9, 10]. There is a dearth of literature on the knowledge of healthcare providers about poisons and their antidotes and the modes and management of poisoning in general in Nigeria. This study set out to document the modes and management of poisoning cases and knowledge of specific antidotes by healthcare providers in selected community pharmacies and hospitals in Lagos state.
Materials and Methods
Study location and population
The study was carried out in Lagos State, Nigeria which has the highest population and largest number of healthcare providers among the other states of the federation [11]. Lagos is the largest cosmopolitan city in Nigeria that accommodates people of different tribes and cultures [12]. It is the largest cosmopolitan city in Nigeria with a rich and diverse culture of many tribes of different states. The study was conducted in two Local Government Areas (LGA) in Lagos State (Ikeja and Surulere LGA) among community pharmacists in registered pharmacies and emergency unit physicians in the secondary and tertiary hospitals. These local governments were chosen based on the location of the two teaching hospitals in the State: the Lagos University Teaching Hospital at Idiaraba, Surulere LGA, and the Lagos State University Teaching Hospital at Ikeja LGA.
Study design
The study was a multicentre, descriptive cross-sectional study among community pharmacists and emergency unit physicians. It was carried out to determine the knowledge and practices of selected healthcare providers about poisoning and its management as a baseline for future studies in this field.
Sampling
Forty community pharmacies were conveniently sampled from each LGA giving a total of 80 pharmacists recruited for the survey. Forty community pharmacies were conveniently selected per area from the list obtained from the Association of Community Pharmacists of Nigeria list for the areas. One pharmacist was chosen per pharmacy. In each LGA, the tertiary hospital and one secondary facility were selected for the survey. Six physicians from each secondary hospital and 10 from each tertiary hospital were chosen to give a total of 32 physicians. In total, 112 pharmacists and physicians (80 pharmacists and 32 physicians) were required for the survey.
Data collection tool
A pre-tested, semi-structured questionnaire was designed to collect relevant data for the study. The questionnaire had four sections: sociodemographic data; respondents’ knowledge and practice, follow-up activities, and poison control activities.
Data collection and analysis
The questionnaire was self-administered. Community pharmacists were approached in their pharmacies and informed consent was obtained before questionnaire administration. At the hospitals, physicians on duty at the emergency unit were approached and informed consent was obtained over two weeks. Respondents that were unable to complete it immediately after administration were given 2 weeks to fill it, after which another 2 weeks was given to mop up any remaining forms. The data obtained were collated and analyzed descriptively as frequencies (percentages), median, and mean as necessary. Inferential statistics were determined using the Student t test. All analyses were carried out with the SPSS version 20.0. P<0.05 were considered statistically significant. Results were presented as frequency tables and charts.
Study outcomes
The outcomes for this study were to document the modes of poisoning cases encountered by the healthcare providers and the usual management of poisoning cases, and finally to determine the knowledge of specific antidotes by healthcare providers. A comparison of the knowledge between the two provider groups studied was also determined. Finally, respondents’ perception of poisoning management in their facilities, availability of poisoning management protocols, and challenges associated with poisoning were additional outcomes.
Results
A total of 96 responses were received, 65 community pharmacists and 31 physicians from the hospitals, giving a response rate of 85.7% (81.3% for the pharmacists and 96.9% for the physicians). All 96 obtained responses were filled and eligible for analysis. Most respondents were female (52.1%) and in the age range of 30-39 years (41.7%); over 83% had had no specialized training on poisoning management. The most common mode of poisoning encountered was accidental (89% and 68% among pharmacists and physicians, respectively) (Table 1).
.jpg)
Contaminated food, alcohol, and kerosene were the agents most commonly implicated in poisoning cases (Table 2).
.jpg)
The majority of the respondents saw less than one poisoning case per month (48.8%) and most of the cases were among children between 0 and 5 years old (41.5% and 48.3% among pharmacists and physicians, respectively). In almost all cases, some form of home remedy or the other had been tried by caregivers (Table 3).
.jpg)
Most of the respondents had poor knowledge about the antidotes to use for different poisons they were presented with. The highest response rate was for antidotes for carbon monoxide and paracetamol (pharmacists at 48% and 46%, respectively; physicians 36% each). Though knowledge was generally poor, pharmacists had a higher mean score than the physicians and the difference in result was statistically significant (P=0.000) (Figures 1 and 2, Table 4).
.jpg)
Referral was the main strategy of management by the pharmacists (33%) while supportive care was the most common strategy utilized by the physicians (61%). Both groups commonly employed specific antidotes (about 42%) (Figure 3). Poisoning management protocols were not available at the facilities surveyed either in the form of guidelines or standard operating procedures/processes or specific antidotes. About 62% of the respondents indicated that poisoning management is inadequate in their facilities (Table 5). The healthcare providers indicated that lack of specific antidotes, required equipment and necessary knowledge were some challenges faced in providing adequate poisoning management (Figure 4). Discussion
This study describes the types and management of poisoning cases and knowledge of specific antidotes by healthcare providers. The study revealed that contaminated food, alcohol, and kerosene were the common agents implicated in poisoning. These agents were followed by household cleaning agents, drugs, and organophosphates. Contaminated food and kerosene may not be surprising as Nigeria has poor access to improved water and sanitation and kerosene is still a major source of fuel for cooking and other household use e.g., as a source of light and heat [13, 14]. These agents were similarly implicated in studies in Enugu, South-Eastern Nigeria, Tanzania, and East Africa [15, 16, 17]. However, studies from other parts of the world reveal that in general, drugs are more common sources of poisoning in the Western world and pesticides in many parts of Asia [18, 19]. The difference in the responses for contaminated food and kerosene were statistically significant between the two groups of respondents.
Demographic details show statistically significant differences in the age range of respondents and years in practice. Most of the respondents are below 40 years of age. The majority of the cases seen by the healthcare providers were accidental though the physicians saw more intentional cases. About half of the accidental cases were in children under 12 with the majority being under 5. Accidental poisoning in children remains a source of concern worldwide but most especially in developing countries [20, 21, 22]. This is a major gap that shows that the education of parents and caregivers in the handling and storage of food and other poisonous items have to be reinforced. The difference in the age group commonly affected by poisoning is statistically significant between the two groups.
There have been more intentional suicide cases among teenagers [23] and this study noted more intentional cases among teenagers similar to a study in Iran where most cases are seen were intentional and among teenagers and young adults (85%) [7, 23]. The difference in the forms of poisoning encountered by respondents is statistically significant.
There are a lot of myths about home-made remedies as antidotes to poisoning but there is a dearth of literature to confirm these claims. Both healthcare providers had heard about home remedies and found that the caregivers had used home management strategies of palm oil, milk, or eggs which are used to initiate vomiting or thought to neutralize the effects of the ingested poison.
Knowledge of antidotes by both pharmacists and physicians was poor even though knowledge gaps varied as shown in previous studies [24, 25]. The difference obtained in this result was statistically significant (P=0.000). This is a gap that needs to be rectified through the training of the various healthcare providers, especially since about four-fifths of the respondents said they had not received any training on poisoning.
The main method of management by the pharmacist was the use of antidotes, referrals, and first aid. Due to their accessibility and skills and services in medication management, they are the first port of call for medical assistance in the community [26]. Management by physicians was supportive of the use of antidotes. This is in line with literature in which supportive care should be the mainstay in poisoning management [27].
The availability of antidotes and poisoning management was generally poor in this study. The majority of the physicians were not aware of the availability of poisoning management protocols in their healthcare facilities, while just under a third of pharmacists said they had guidelines for the management of standard operating procedures. The difference in the availability of poisoning management protocol in the facility is statistically significant between the two groups of respondents. The main challenges faced were a lack of antidotes, adequate equipment, and knowledge. As expected, activated charcoal was largely available, especially in the community pharmacies. The unavailability of antidotes in healthcare facilities has been widely reported by other studies [25, 28, 29, 30].
The need for a poison control center was recognized by most respondents in this study with most feeling that poison cases should be reported to a central poison center. Other studies also recognized the importance of poison control centers [2, 31, 32, 33, 34]. A previous study showed that establishing poison information centers in different parts of the country, preparing national treatment guidelines, training healthcare providers, and ensuring the availability of, and easy access to antidotes were the issues that must be solved to ensure proper management of poisoning in healthcare facilities. Other proposed solutions include education on the importance of stocking antidotes, regular review of storage of antidotes, development of distribution plans, and the development of antidote guidelines. Future research to improve the management of poisoning was also recommended [25, 28, 29, 30, 31, 32, 33, 34].
The study was limited to two locations which were conveniently chosen and sampled healthcare providers hence the results may not be generalizable though it provides useful information for planning and further studies, especially among community pharmacists and physicians.
Knowledge of antidotes to various poisons was poor and management of poisoning was largely inadequate. The establishment of poison control centers in healthcare facilities and the organization of updated lectures and training for community pharmacists and physicians will go a long way to improving poisoning management in the state.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Lagos University Teaching Hospital (LUTH) Research and Ethics Committee. Approval to use facilities was obtained from the individual hospitals, as well as the Association of Community Pharmacists of Nigeria (ACPN), Lagos State Branch.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology: Arinola Joda, Oluwaseun Ajetunmobi; Investigation, writing – review & editing: All authors; Writing – original draft: Arinola Joda, Olubusola Olugbake.
Conflict of interest
The authors declare no conflict of interest associated with this study.
References
- WHO 2018. International Programme on Chemical Safety: Poisoning Prevention and Management. Available at: http://www.who.int/ipcs/poisons/en/. Accessed 26th March 2020
- Crouch R, Charters A and Bennett P. Emergency nursing. In: Oxford Handbook of Emergency Nursing. 2nd edition. Oxford: Oxford University Press; 2016. [DOI:10.1093/med/9780199203499.001.0001]
- Jesslin J, Adepu R, Churi S. Assessment of prevalence and mortality incidences due to poisoning in a South Indian Tertiary Care Teaching Hospital. Indian J Pharm Sci. 2010; 72(5):587-91. [DOI:10.4103/0250-474X.78525] [PMID] [PMCID]
- World Health Organization (WHO). World Health Statistics: Overview 2019. [Accessed: 2020 March 27]. Available at: https://apps.who.int/iris/bitstream/handle/10665/311696/WHO-DAD-2019.1-eng.pdf
- Akubue PI. Poisons in our environment and drug overdose: A guide for health professionals and the lay public. New York: P.I. Akubue; 1997. https://www.bookdepository.com/Poisons-Our-Environment-Drug-Overdose-P-Iwe-Akubue/9789782897060
- Henry JA, Wiseman HM. Management of poisoning: A handbook for health care workers. World Health Organization & International Programme on Chemical Safety. 1997. [Accessed: 2020 March 20]. Available at: https://apps.who.int/iris/handle/10665/41991
- Ahmadi A, Pakravan N, Ghazizadeh Z. Pattern of acute food, drug, and chemical poisoning in Sari City, Northern Iran. Hum Exp Toxicol. 2010; 29(9):731-8. [DOI:10.1177/0960327110361501] [PMID]
- Whyte IM, Dawson AH, Buckley NA, Carter GL, Levey CM. Health care: A model for the management of self‐poisoning. Med J Aust. 1997; 167(3):142-6. [DOI:10.5694/j.1326-5377.1997.tb138813.x] [PMID]
- Koce F, Randhawa G, Ochieng B. Understanding healthcare self-referral in Nigeria from the service users’ perspective: A qualitative study of Niger state. BMC Health Serv Res. 2019; 19(1):209. [DOI:10.1186/s12913-019-4046-9] [PMID] [PMCID]
- Ogbo PU, Aina BA, Aderemi-Williams RI. Management of acute diarrhoea in children by community pharmacists in Lagos, Nigeria. Pharm Pract. 2014; 12(1):376. [DOI:10.4321/S1886-36552014000100002] [PMID] [PMCID]
- World Population Review. Lagos state Population. 2018. [Accessed on 31st January 2019]. Available at: http://worldpopulationreview.com/world-cities/lagos-population/.
- Adedun E, Shodipe M. Yoruba-English bilingualism in central Lagos - Nigeria. J African Cult Stud. 2011; 23(2):121-32. [DOI:10.1080/13696815.2011.637882]
- UNICEF report. Nigeria-Water, Sanitation and Hygiene 2018. [Accessed: 2020 31st January]. Available at https://www.unicef.org/nigeria/water-sanitation-and-hygiene
- Folayan, MO, Obiyan, MO, Olaleye AO. Association between water, sanitation, general hygiene and oral hygiene practices of street-involved young people in Southwest Nigeria. BMC Oral Health. 2020; 20(1):32. [DOI:10.1186/s12903-020-1022-z] [PMID] [PMCID]
- Edelu BO, Odetunde OI, Eke CB, Uwaezuoke NA, Oguonu T. Accidental Childhood poisoning in Enugu, South-East, Nigeria. Ann Med Health Sci Res. 2016; 6(3):168-71. [DOI:10.4103/2141-9248.183944] [PMID] [PMCID]
- Mbarouk GS, Sawe HR, Mfinanga JA, Stein J, Levin S, Mwafongo V, et al. Patients with acute poisoning presenting to an urban emergency department of a tertiary hospital in Tanzania. BMC Res Notes. 2017; 10(1):482. [DOI:10.1186/s13104-017-2807-2] [PMID] [PMCID]
- Tagwireyi D, Chingombe P, Khoza S, Maredza M. Pattern and epidemiology of poisoning in the East African Region: A literature review. J Toxicol. 2016; 2016:8789624. [DOI:10.1155/2016/8789624] [PMID] [PMCID]
- Fingerhut LA, Cox CS. Poisoning mortality, 1985-1995. Public Health Rep. 1998; 113(3):218-33. [PMID] [PMCID]
- Singh O, Javeri Y, Juneja D, Gupta M, Singh G, Dang R. Profile and outcome of patients with acute toxicity admitted in intensive care unit: Experiences from a major corporate hospital in urban India. Indian J Anaesth. 2011; 55(4):370-4. [DOI:10.4103/0019-5049.84860] [PMID] [PMCID]
- Oguche S, Bukbuk DN, Watila IM. Pattern of hospital admissions of children with poisoning in the Sudano-Sahelian North Eastern Nigeria. Niger J Clin Pract. 2007; 10(2):111-5. [PMID]
- Sleet DA. The global challenge of child injury prevention.Int J Environ Res Public Health. 2018; 15(9):1921. [DOI:10.3390/ijerph15091921] [PMID] [PMCID]
- Dayasiri MBKC, Jayamanne SF, Jayasinghe CY. Risk factors for acute unintentional poisoning among children aged 1-5 years in the rural community of Sri Lanka. Int J Pediatr. 2017; 2017:4375987. [DOI:10.1155/2017/4375987] [PMID] [PMCID]
- Spiller HA, Ackerman JP, Smith GA, Kistamgari S, Funk AR, McDermott MR, et al. Suicide attempts by self-poisoning in the United States among 10-25-year olds from 2000 to 2018: Substances used, temporal changes and demographics. J Clin Toxicol (Philadelphia, Pa.). 2020; 58(7):676-87. [DOI:10.1080/15563650.2019.1665182] [PMID]
- Lidder S, Ovaska H, Archer JR, Greene SL, Jones AL, Dargan PI, et al. Doctors’ knowledge of the appropriate use and route of administration of antidotes in the management of recreational drug toxicity. Emerg Med J. 2008; 25:820-3. [DOI:10.1136/emj.2007.054890] [PMID]
- Arslan N, Khiljee S, Bakhsh A, Ashraf M , Maqsood I. Availability of antidotes and key emergency drugs in tertiary care hospitals of Punjab and assessment of the knowledge of health care professionals in the management of poisoning cases. Pak J Pharm Sci. 2016; 29(2):603-7. https://applications.emro.who.int/imemrf/Pak_J_Pharm_Sci/Pak_J_Pharm_Sci_2016_29_2_603_607.pdf
- Lan SM, Oreagba IA, Usman SO, Oparah AC. Willingness to practice basic first aid care among community pharmacists in Lagos Nigeria. West African J Pharm. 2012; 23(2):73-83. http://www.wapharm.org/wajp/admin/12389900798187/73-83.pdf
- Albertson T, Owen KP, Sutter ME, Chan AL. Gastrointestinal decontamination in the acutely poisoned patient. Int J Emerg Med. 2011; 4:65. [DOI:10.1186/1865-1380-4-65] [PMID] [PMCID]
- Nissen LM, Wong KH, Jones A, Roberts DM. Availability of antidotes for the treatment of acute poisoning in Queensland public hospitals. Aust J Rural Health. 2010; 18(2):78-84. [DOI:10.1111/j.1440-1584.2010.01129.x] [PMID]
- Al-Sohaim SI, Awang R, Zyoud SH, Rashid SM, Hashim S. Evaluate the impact of hospital types on the availability of antidotes for the management of acute toxic exposures and poisonings in Malaysia. Hum Exp Toxicol. 2012; 31(3):274-81. [DOI:10.1177/0960327111405861] [PMID]
- Al-Taweel D, Al-Haqan A, Qabazard B, Abuzainah D, Koshy S, Alqenae F, et al. Availability of antidotes in Kuwait: A national audit. J Emerg Med. 2019; 58(2):305-12. [DOI:10.1016/j.jemermed.2019.11.016] [PMID]
- Blizzard JC, Michels JE, Richardson WH, Reeder CE, Schulz RM, Holstege CP. Cost-benefit analysis of a regional poison center. Clin Toxicol (Philadelphia, Pa.). 2008; 46(5):450-6 [DOI:10.1080/15563650701616145] [PMID]
- Burki TK. Nigeria’s lead poisoning crisis could have a long legacy. Lancet. 2012; 379(9818):792. [DOI:10.1016/S0140-6736(12)60332-8]
- Elamin ME, James DA, Holmes P, Jackson G, Thompson JP, Sandilands EA, et al. Reductions in emergency department visits after primary healthcare use of the UK National Poisons Information Service. Clin Toxicol (Philadelphia, Pa.). 2018; 56(5):342-7. [DOI:10.1080/15563650.2017.1390120] [PMID]
- Wang A, Law R, Lyons R, Choudhary E, Wolkin A, Schier J. Assessing the public health impact of using poison center data for public health surveillance. Clin Toxicol (Philadelphia, Pa.). 2018; 56(7):646-52. [DOI:10.1080/15563650.2017.1413194] [PMID] [PMCID]
Type of Study: Original Research |
Subject:
Toxicology
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








.jpg)
.jpg)

