Volume 6, Issue 2 (2020)
Pharm Biomed Res 2020, 6(2): 143-150 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Islam S, Sohan M, Ahmed F, Nahar Z, Rabiul Islam M. Evaluation of the Pharmacotherapeutic Pattern for Treating Schizophrenia in Bangladesh. Pharm Biomed Res 2020; 6 (2) :143-150
URL: http://pbr.mazums.ac.ir/article-1-289-en.html
URL: http://pbr.mazums.ac.ir/article-1-289-en.html
1- Department of Pharmacy, University of Asia Pacific, 74/A Green Road, Farmgate, Dhaka-1205, Bangladesh.
Full-Text [PDF 705 kb]
(1329 Downloads)
| Abstract (HTML) (3313 Views)
Full-Text: (2273 Views)
Introduction
Schizophrenia is a highly disabling and debilitating disorder. It is considered one of the most serious and frightening mental illnesses that afflict about 1% of the population. The disease is characterized by abnormal behavior, profound disruptions in thinking, disorganized speech, and a decreased ability to understand reality [1, 2]. The disease boundaries have remained unclear due to substantial overlap with other psychotic disorders [1]. It is also characterized by delusion, hallucinations, and impaired cognitive functions [3]. Schizophrenia is not a unitary disorder and at its early prodromal stage, it is indistinguishable from a mood disorder [4]. According to a recent systematic literature review, from 1990 to 2013, the median estimate of schizophrenia prevalence in 29 studies was 0.48%, with an interquartile range of 0.34% to 0.85% [5]. A 2008 study reported a median incidence of schizophrenia of 15.2 per 100000 persons, with the central 80% of estimates varying over a five-fold range from 7.7 to 43.0 per 100000 persons [6].
The inherent heterogeneity of schizophrenia manifestation has resulted in a lack of consensus over the disorder’s diagnostic criteria, etiology, and pathophysiology [3]. Most theories focus on either an excess or a deficiency of neurotransmitters (notably dopamine, serotonin, and glutamate) providing consequential influence on the pathophysiology of schizophrenia. Other theories implicate aspartate, glycine, and gamma-aminobutyric acid as part of the neurochemical imbalance in schizophrenia [3]. Genetic susceptibility and early developmental impairments are the major contributing factors for developing schizophrenia.
One of the most well-established findings in schizophrenia research was that vulnerability to the illness can be inherited [7]. It has been found that the rate of schizophrenia and other mental illnesses, in the biological offspring of parents with schizophrenia is higher when compared to adoptees with no mental illness in biological parents [8]. It has been observed that approximately 6.6% of all first-degree relatives of the patients are affected. If both parents are affected, the risk of disease for offspring sharply elevates to 40%. The concordance rate for monozygotic twins is 50%, compared to 10% for dizygotic twins. Schizophrenia-prone families are also at risk for other psychiatric disorders. Therefore, consensus indicates that multiple factors, including genetic susceptibility and environmental factors, contribute to the varied phenotypes manifested in this ailment [9, 10].
According to WHO, the number of people with schizophrenia around the world can be estimated at 29 million, of whom around 20 million live in developing or least developed countries. Surveys have been carried out in various countries where the prevalence of schizophrenia was between 0.1 and 0.4 per 1000 population in adults [11]. In Bangladesh, 30% of the patients who are treated in psychiatric outpatient facilities are primarily diagnosed with schizophrenia. In community-based psychiatric inpatient admission, 42% are primarily diagnosed with schizophrenia [12]. Despite the high prevalence and a large number of schizophrenic patients, we do not have any reported studies regarding the pharmacotherapeutic pattern from Bangladesh. This type of study will provide confidence to the physicians for selecting the right medications for schizophrenic patients. The present study aimed to investigate the actual drug usage among Bangladeshi schizophrenic patients and to compare it with the standard prescribing guidelines to determine any inconsistencies. We also try to find out the sociodemographic pattern of schizophrenic patients in Bangladesh.
Materials and Methods
This survey-based study was carried out for six months at the National Institute of Mental Health (NIMH), Dhaka, Bangladesh and Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka Bangladesh. The aforementioned institutes serve as a referral center for patients requiring specialized mental care and the patient population encompasses a wide income range and demographic background. A structured questionnaire was developed and validated through multi-stage cross-referencing by authorized pharmacists. Informed consent was taken from the patients’ guardians regarding the questionnaire. Patients were diagnosed by qualified psychiatrists according to the diagnostic criteria of DSM-5 (the diagnostic and statistical manual of mental disorders, 5th edition). In Bangladesh, approximately 3.4 million people suffer from schizophrenia. It was assumed that confidence level, the margin of error, and response distribution will be 95%, 5%, and 80%, respectively. According to this assumption, the approximate sample size was supposed to be 246 and finally, a total of 250 patients were included in the present study [13, 14].
Patients with other comorbid psychiatric illness and mental retardation were excluded from this study. Physicians confirmed the participants as cases who were suffering from schizophrenic symptoms for at least two weeks. The attendants of all participated patients were inquired and their prescriptions were verified to obtain pharmacotherapeutic data and other necessary information. A major focus of this study was to investigate the pattern of pharmacotherapy and find the frequency of specific classes of drugs prescribed in the treatment of schizophrenia. SPSS version 23.0 (IBM SPSS Statistics for Windows, Version 23.0, Armonk, NY) was used for all statistical analyses.
The study was approved by the ethical review committee of the participating organizations. All investigations were performed according to the principles stated in the Declaration of Helsinki (Version 2008, Seoul, Korea). The objective of the study was well briefed to the caregivers of all patients and written consent was obtained. The guardians who denied consent after facing the questionnaire were also excluded from this study.
Results
Demographic characteristics of the patients
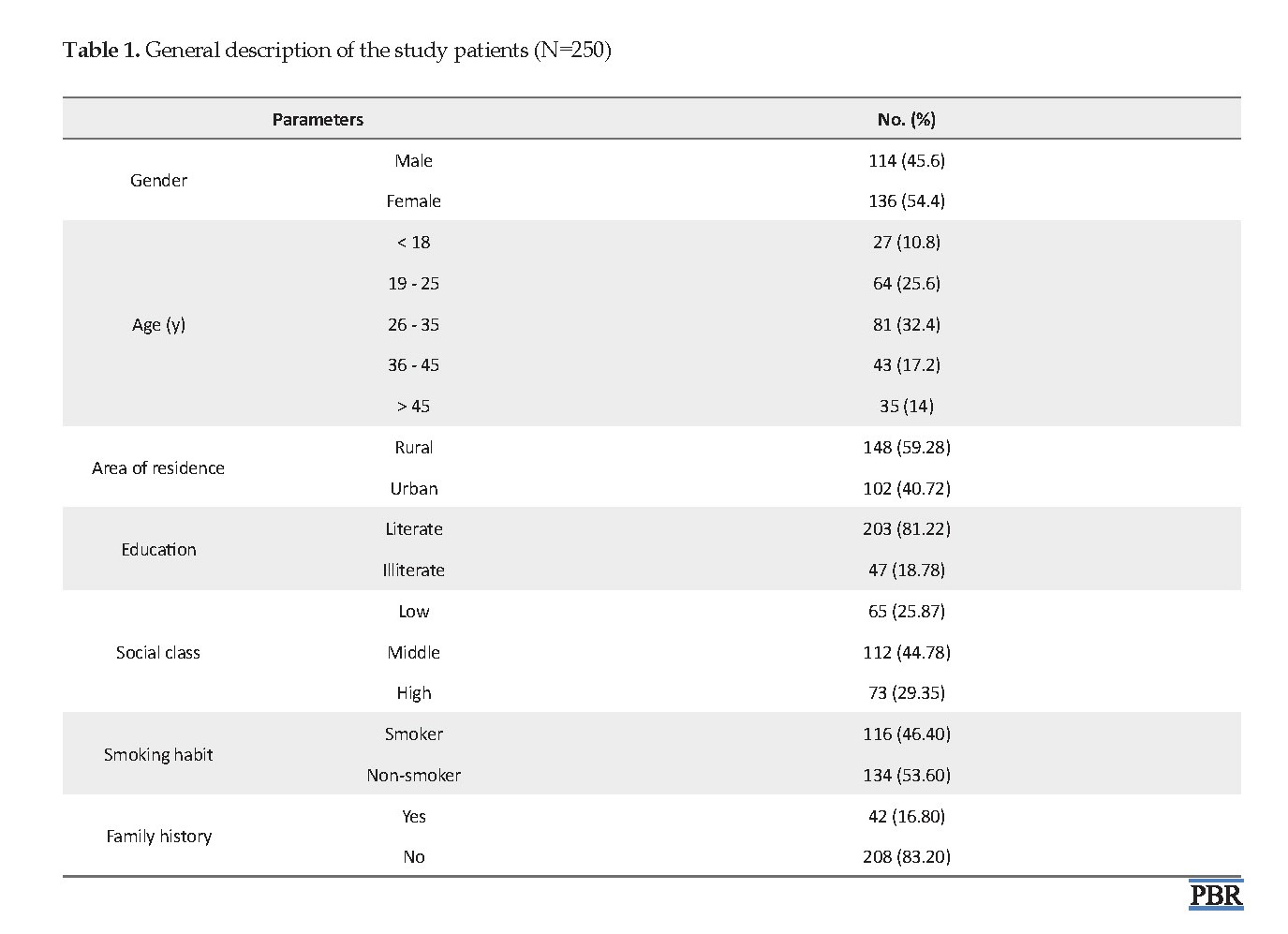
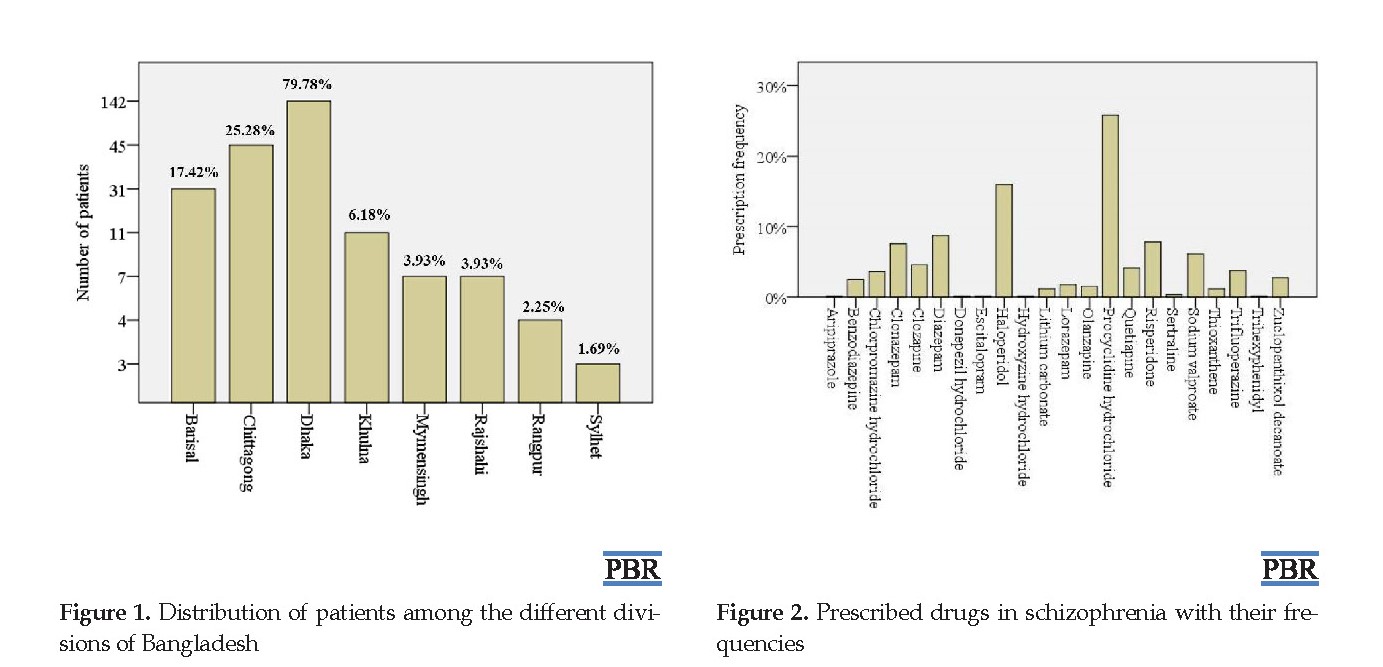
Out of 250 patients from NIMH and BSMMU (Table 1), the frequency of females (n=136, 54.4%) was higher than males (n=114, 45.6%). In our study, we divided schizophrenic patients into different age groups to find the association of schizophrenia with the patient’s age. The risk for developing schizophrenia increases with older age and our study indicates that 63.6% of patients suffering from schizophrenia were older than 25 years. According to this study, 79.78% of patients were from the Dhaka region followed by Chittagong (25.28%). This study reported the highest number of schizophrenic patients from the middle economic class (44.78%) followed by the higher economic class (29.35%). We also found that the number of schizophrenic patients was higher in rural areas (n=148, 59.28%) compared with the urban areas. Moreover, we observed that 16.80% of schizophrenic patients had schizophrenia among their first degree relatives. Sociodemographic profiles of patients were presented in Table 1 and Figure 1.
The pattern of pharmacotherapy
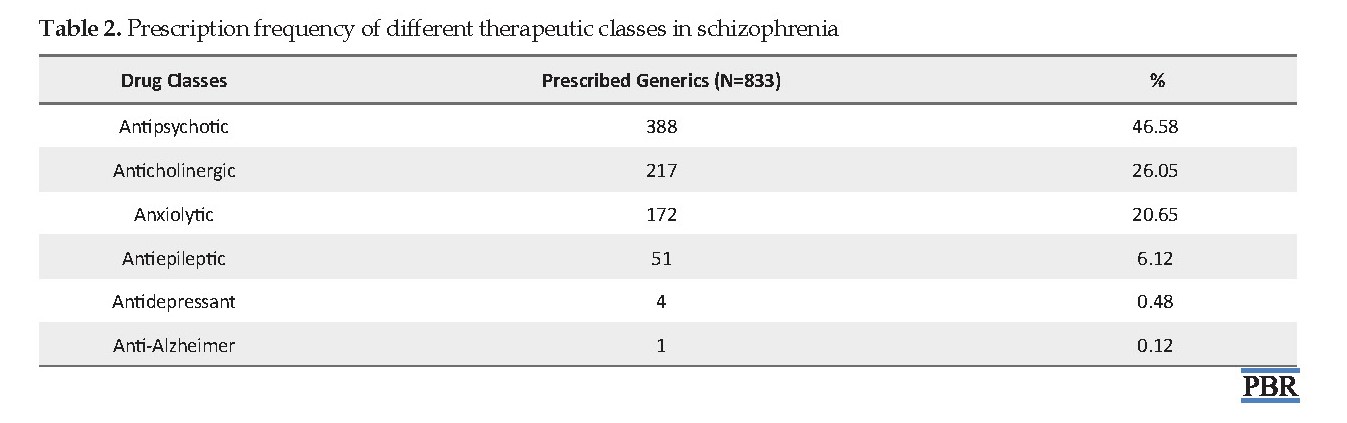
We observed that all the prescriptions contained multiple medications. The study revealed that the highest use of treatment drugs belonged to the antipsychotics (n=388, 46.58%) followed by anticholinergic (n=217, 26.05%) and anxiolytic drugs (n=172, 20.65%) as shown in Table 2. Most prescriptions contained a combination of drugs belonging to some specific therapeutic categories, specifically, antipsychotic, antidepressant, anticholinergic, and anxiolytic drugs (Figure 2). Procyclidine hydrochloride was the highest among all prescribed generics as an anticholinergic agent (n=215, 25.81%). In the case of antipsychotic agents, the prescribing rate of haloperidol (n=133, 15.97%) and clozapine (n=63, 7.56%) were high. Anticonvulsant drug therapy was frequently prescribed to patients suffering from schizophrenia. The only one anti-Alzheimer drug prescribed was donepezil hydrochloride. Diazepam was the most frequently prescribed generic as an anxiolytic agent (n=73, 8.76%). In the present survey, approximately 80% of prescriptions were collected from the inpatient department. The combination of haloperidol and procyclidine hydrochloride was common for those cases. Frequent use of either clonazepam or diazepam with procyclidine hydrochloride was also noticed. On the other hand, single-drug was predominantly prescribed to treat schizophrenia in the outpatient department.
Discussion
Studies regarding the investigation of the pharmacotherapeutic pattern on schizophrenic patients are not very common in our country. However, such studies will allow an in-depth exploration of the health problem and provide a better understanding of pharmacotherapy. It will also help us to compare the pharmacotherapeutic pattern of Bangladeshi schizophrenic patients with the standard guidelines and recommendations.
Schizophrenia is a highly disabling and debilitating disorder. It is considered one of the most serious and frightening mental illnesses that afflict about 1% of the population. The disease is characterized by abnormal behavior, profound disruptions in thinking, disorganized speech, and a decreased ability to understand reality [1, 2]. The disease boundaries have remained unclear due to substantial overlap with other psychotic disorders [1]. It is also characterized by delusion, hallucinations, and impaired cognitive functions [3]. Schizophrenia is not a unitary disorder and at its early prodromal stage, it is indistinguishable from a mood disorder [4]. According to a recent systematic literature review, from 1990 to 2013, the median estimate of schizophrenia prevalence in 29 studies was 0.48%, with an interquartile range of 0.34% to 0.85% [5]. A 2008 study reported a median incidence of schizophrenia of 15.2 per 100000 persons, with the central 80% of estimates varying over a five-fold range from 7.7 to 43.0 per 100000 persons [6].
The inherent heterogeneity of schizophrenia manifestation has resulted in a lack of consensus over the disorder’s diagnostic criteria, etiology, and pathophysiology [3]. Most theories focus on either an excess or a deficiency of neurotransmitters (notably dopamine, serotonin, and glutamate) providing consequential influence on the pathophysiology of schizophrenia. Other theories implicate aspartate, glycine, and gamma-aminobutyric acid as part of the neurochemical imbalance in schizophrenia [3]. Genetic susceptibility and early developmental impairments are the major contributing factors for developing schizophrenia.
One of the most well-established findings in schizophrenia research was that vulnerability to the illness can be inherited [7]. It has been found that the rate of schizophrenia and other mental illnesses, in the biological offspring of parents with schizophrenia is higher when compared to adoptees with no mental illness in biological parents [8]. It has been observed that approximately 6.6% of all first-degree relatives of the patients are affected. If both parents are affected, the risk of disease for offspring sharply elevates to 40%. The concordance rate for monozygotic twins is 50%, compared to 10% for dizygotic twins. Schizophrenia-prone families are also at risk for other psychiatric disorders. Therefore, consensus indicates that multiple factors, including genetic susceptibility and environmental factors, contribute to the varied phenotypes manifested in this ailment [9, 10].
According to WHO, the number of people with schizophrenia around the world can be estimated at 29 million, of whom around 20 million live in developing or least developed countries. Surveys have been carried out in various countries where the prevalence of schizophrenia was between 0.1 and 0.4 per 1000 population in adults [11]. In Bangladesh, 30% of the patients who are treated in psychiatric outpatient facilities are primarily diagnosed with schizophrenia. In community-based psychiatric inpatient admission, 42% are primarily diagnosed with schizophrenia [12]. Despite the high prevalence and a large number of schizophrenic patients, we do not have any reported studies regarding the pharmacotherapeutic pattern from Bangladesh. This type of study will provide confidence to the physicians for selecting the right medications for schizophrenic patients. The present study aimed to investigate the actual drug usage among Bangladeshi schizophrenic patients and to compare it with the standard prescribing guidelines to determine any inconsistencies. We also try to find out the sociodemographic pattern of schizophrenic patients in Bangladesh.
Materials and Methods
This survey-based study was carried out for six months at the National Institute of Mental Health (NIMH), Dhaka, Bangladesh and Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka Bangladesh. The aforementioned institutes serve as a referral center for patients requiring specialized mental care and the patient population encompasses a wide income range and demographic background. A structured questionnaire was developed and validated through multi-stage cross-referencing by authorized pharmacists. Informed consent was taken from the patients’ guardians regarding the questionnaire. Patients were diagnosed by qualified psychiatrists according to the diagnostic criteria of DSM-5 (the diagnostic and statistical manual of mental disorders, 5th edition). In Bangladesh, approximately 3.4 million people suffer from schizophrenia. It was assumed that confidence level, the margin of error, and response distribution will be 95%, 5%, and 80%, respectively. According to this assumption, the approximate sample size was supposed to be 246 and finally, a total of 250 patients were included in the present study [13, 14].
Patients with other comorbid psychiatric illness and mental retardation were excluded from this study. Physicians confirmed the participants as cases who were suffering from schizophrenic symptoms for at least two weeks. The attendants of all participated patients were inquired and their prescriptions were verified to obtain pharmacotherapeutic data and other necessary information. A major focus of this study was to investigate the pattern of pharmacotherapy and find the frequency of specific classes of drugs prescribed in the treatment of schizophrenia. SPSS version 23.0 (IBM SPSS Statistics for Windows, Version 23.0, Armonk, NY) was used for all statistical analyses.
The study was approved by the ethical review committee of the participating organizations. All investigations were performed according to the principles stated in the Declaration of Helsinki (Version 2008, Seoul, Korea). The objective of the study was well briefed to the caregivers of all patients and written consent was obtained. The guardians who denied consent after facing the questionnaire were also excluded from this study.
Results
Demographic characteristics of the patients
Out of 250 patients from NIMH and BSMMU (Table 1), the frequency of females (n=136, 54.4%) was higher than males (n=114, 45.6%). In our study, we divided schizophrenic patients into different age groups to find the association of schizophrenia with the patient’s age. The risk for developing schizophrenia increases with older age and our study indicates that 63.6% of patients suffering from schizophrenia were older than 25 years. According to this study, 79.78% of patients were from the Dhaka region followed by Chittagong (25.28%). This study reported the highest number of schizophrenic patients from the middle economic class (44.78%) followed by the higher economic class (29.35%). We also found that the number of schizophrenic patients was higher in rural areas (n=148, 59.28%) compared with the urban areas. Moreover, we observed that 16.80% of schizophrenic patients had schizophrenia among their first degree relatives. Sociodemographic profiles of patients were presented in Table 1 and Figure 1.
The pattern of pharmacotherapy
We observed that all the prescriptions contained multiple medications. The study revealed that the highest use of treatment drugs belonged to the antipsychotics (n=388, 46.58%) followed by anticholinergic (n=217, 26.05%) and anxiolytic drugs (n=172, 20.65%) as shown in Table 2. Most prescriptions contained a combination of drugs belonging to some specific therapeutic categories, specifically, antipsychotic, antidepressant, anticholinergic, and anxiolytic drugs (Figure 2). Procyclidine hydrochloride was the highest among all prescribed generics as an anticholinergic agent (n=215, 25.81%). In the case of antipsychotic agents, the prescribing rate of haloperidol (n=133, 15.97%) and clozapine (n=63, 7.56%) were high. Anticonvulsant drug therapy was frequently prescribed to patients suffering from schizophrenia. The only one anti-Alzheimer drug prescribed was donepezil hydrochloride. Diazepam was the most frequently prescribed generic as an anxiolytic agent (n=73, 8.76%). In the present survey, approximately 80% of prescriptions were collected from the inpatient department. The combination of haloperidol and procyclidine hydrochloride was common for those cases. Frequent use of either clonazepam or diazepam with procyclidine hydrochloride was also noticed. On the other hand, single-drug was predominantly prescribed to treat schizophrenia in the outpatient department.
Discussion
Studies regarding the investigation of the pharmacotherapeutic pattern on schizophrenic patients are not very common in our country. However, such studies will allow an in-depth exploration of the health problem and provide a better understanding of pharmacotherapy. It will also help us to compare the pharmacotherapeutic pattern of Bangladeshi schizophrenic patients with the standard guidelines and recommendations.
According to one of the WHO collaborative studies, the number of schizophrenic patients was higher among males. WHO included a total of 452474 patients in that study and the male/female ratio was 150969/116459. The number of male patients from urban and rural areas was 118971 and 31998, respectively. Out of 116459 female patients, 86815 were residing in urban areas and 29644 in rural areas [15]. In developed countries, no significant difference exists between males and females or between urban and rural [16]. In our study, we found that most schizophrenic patients were female residing in rural areas. This finding may be due to the overall status of women in south Asian rural areas. The 1998 world health report states that women’s mental health is inextricably linked to their status in society [17]. Woman in our rural society suffers from discrimination; mentally ill women have more pregnancy and childbirth-related complications [18].
The study revealed no consistent sex difference for different age groups in either the urban or the rural cohort in India [19]. A tendency to earlier onset in males with a peak incidence in the early twenties in contrast with the late twenties or early thirties in females has been consistently asserted [20]. In our study, we found the highest frequency of patients among those older than 25 years. Also, the influence of social class has been found as a high percentage of patients were from the lower middle class compared with the upper classes.
According to the present study, we observed the rate of schizophrenic attacks was more in the educated population with middle economic status residing in rural areas. The factors that differentiate the mental health conditions of different social classes could be the availability of suitable jobs, supportive family attitudes, and extended family as suggested by several studies [21].
Pharmacotherapy is given to the patients according to the severity of the disease and associated complications. Pharmacotherapy involves drugs from different categories like antipsychotics, antidepressants, and anticonvulsants, and so on for treating different kinds of hallucinations, inducing schizophrenia (e.g. auditory, visual, olfactory, gustatory, etc.) [22]. For patients suffering from schizophrenia, the antipsychotic medication should be recommended as the first line of treatment. According to the American Psychiatric Association (APA), second-generation (atypical) Antipsychotics (SGAs) except clozapine are the agents of choice for the first-line treatment of schizophrenia. Clozapine is not recommended because of its risk of agranulocytosis [23]. Moreover, clozapine was found to be more effective than haloperidol for treating schizophrenia [24]. In our study, we observed that the first-generation antipsychotic agents are used almost twice more frequently than the second-generation agents in the treatment of schizophrenia in Bangladesh. Haloperidol is the most used first-generation agent. According to the 6-stage pharmacotherapeutic algorithm for the treatment of schizophrenia by the Texas Medication Algorithm Project (TMAP), stage 1 is the first-line monotherapy with an SGA. If the patient shows little or no response, he or she should proceed to the next stage which consists of monotherapy with either another SGA or First-Generation Antipsychotics (FGA). If there is still no response, the patient should move to stage 3, where clozapine monotherapy with monitoring of the White Blood Cell (WBC) count is suggested. If agranulocytosis arises, clozapine should be stopped. The patient should proceed to stage 4 in combination with clozapine and FGA or SGA, and or Electroconvulsive Therapy (ECT) if stage 3 therapy fails to give a positive response. If no treatment response is still observed from stage 4, monotherapy with an FGA or an SGA (that has not been tried) should be applied. Finally, stage 6 consists of combination therapy with an SGA, an FGA, ECT, and or a mood stabilizer if stage 5 treatment is unsuccessful [25-27]. We observed the use of the antiepileptic drug for some patients as a combination where the first three stages failed. No inconsistencies have been shown with the guidelines given by APA and TMAP.
It was observed that anticholinergic drugs, like procyclidine hydrochloride, are widely used in Bangladesh possibly to minimize the extrapyramidal side effects of antipsychotics. Anticholinergic drugs are being prescribed for symptomatic treatment of Parkinson disease for over a century and they are still trusted by physicians. For patients with psychosis and schizophrenia, anticholinergics are primarily used to counter the extrapyramidal side effects or prevent side effects induced by antipsychotics [28]. Extrapyramidal side effects such as Parkinsonism are believed to be the unavoidable result of antipsychotic efficacy conferred by dopamine D2 receptor blockade [29]. However, they can cause distressing peripheral side-effects (e.g. dry mouth and constipation) and CNS adverse effects (e.g. cognitive impairment, worsening of tardive dyskinesia, and delirium) [30].
We found that antidepressants were often prescribed to patients suffering from depression. Moreover, we observed that anxiolytics are prescribed to the patients suffering from debilitating anxiety to induce sedation. Benzodiazepines are the most widely prescribed anxiolytics in Bangladesh and are more effective than barbiturates and meprobamate [31]. Treatment with benzodiazepines may target a novel therapeutic mechanism beyond the scope of traditional antipsychotics. The present study has some limitations, for example, the severity of the disease, the duration of treatment, patient type (old or new), rate of antipsychotic combination therapy, and failure with previous treatment have not been reported.
We revealed the prescription pattern and demographic trend of schizophrenia in Bangladesh for the first time using large datasets. The study indicates antipsychotics and anticholinergics are the major drugs prescribed for treating schizophrenia. Besides, the first and second generations of antipsychotics are also prescribed in such a way that it complies with the authorized and established guidelines throughout the world. The present study findings will be helpful to physicians for treating schizophrenic patients.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the ethical review committee of the participating organizations. All investigations were performed according to the principles stated in the Declaration of Helsinki (Version 2008, Seoul, Korea).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and methodology: Zabun Nahar, Md. Rabiul Islam; Conduction, analysis, and initial draft writing: Salsabil Islam, Md. Sohan, Faysal Ahmed; Revise and editing of manuscript: Md. Rabiul Islam, Salsabil Islam, Md. Sohan; Supervision: Zabun Nahar, Md. Rabiul Islam; All authors reviewed and approved the final version of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We acknowledge the National Institute of Mental Health (NIMH), Dhaka, Bangladesh, and Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka Bangladesh for their administrative support, facilities, and instrumentations.
References
World Health Organization. Schizophrenia [Internet]. 2019 [Updated 4 October 2019]. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia
National Institute of Mental Health. Schizophrenia [Internet]. 2020 [Updated 10 May 2020]. Available from: https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml
Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. P & T. 2014; 39(9):638-45. [PMID] [PMCID]
Fountoulakis KN, Popovic D, Mosheva M, Siamouli M, Moutou K, Gonda X. Mood symptoms in stabilized patients with schizophrenia: A bipolar type with predominant psychotic featuews? Psychiatr Danub. 2017; 29(2):148-54.[DOI:10.24869/psyd.2017.148] [PMID]
Wu Y, Kang R, Yan Y, Gao K, Li Z, Jiang J, et al. Epidemiology of schizophrenia and risk factors of schizophrenia-associated aggression from 2011 to 2015. J Int Med Res. 2018; 46(10):4039-49. [DOI:10.1177/0300060518786634] [PMID] [PMCID]
McGrath J, Saha S, Chant D, Welham J. Schizophrenia: A concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008; 30:67-76. [DOI:10.1093/epirev/mxn001] [PMID]
Gejman PV, Sanders AR, Duan J. The role of genetics in the etiology of schizophrenia. Psychiatr Clin North Am. 2010; 33(1):35-66. [DOI:10.1016/j.psc.2009.12.003] [PMID] [PMCID]
Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: A meta-analysis of family high-risk studies. Schizophr Bull. 2013; 40(1):28-38. [DOI:10.1093/schbul/sbt114] [PMID] [PMCID]
Nishuty NL, Khandoker MMH, Karmoker JR, Ferdous S, Shahriar M, Qusar MMAS, et al. Evaluation of serum interleukin-6 and C-reactive protein levels in Drug-naïve major depressive disorder patients. Cureus. 2019; 11(1):e3868.. [DOI:10.7759/cureus.3868] [PMID] [PMCID]
Kim YK, Na KS, Myint AM, Leonard BE. The role of pro-inflammatory cytokines in neuroinflammation, neurogenesis and the neuroendocrine system in major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2016; 64:277-84. [DOI:10.1016/j.pnpbp.2015.06.008] [PMID]
Barbato A. Schizophrenia and public health [Internet]. 1998 [Updated 1998] Available from: https://www.who.int/mental_health/media/en/55.pdf
World Health Organization. WHO-aims report on mental health system in Bangladesh: A report of the assessment of the mental health system in Bangladesh using the World Health Organization - assessment instrument for mental health systems (WHO-AIMS) [Internet]. 2007 [Updated 2007]. Available from: https://www.who.int/mental_health/bangladesh_who_aims_report.pdf
Goetghebeur E. Book reviews: Lemeshow S, Homser DW Jr, Klar J, Lwanga SK 1990: Adequacy of sample size in health studies. Chichester: John Wiley & Sons for WHO. Stat Methods Med Res. 1992; 1(1):120. [DOI:10.1177/096228029200100108]
Didar Hossain M, Ahmed HََU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: A systematic review. BMC Psychiatry. 2014; 14:216. [DOI:10.1186/s12888-014-0216-9] [PMID] [PMCID]
Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of Schizophrenia. PLoS Med. 2005; 2(5):e141. [DOI:10.1371/journal.pmed.0020141] [PMID] [PMCID]
Hamza A, Sharma MK, Anand N, Marimuthu P, Thamilselvan P, Thakur PC, et al. Urban and rural pattern of Internet use among youth and its association with mood state. J Family Med Prim Care. 2019; 8(8):2602-6. [DOI:10.4103/jfmpc.jfmpc_428_19] [PMID] [PMCID]
Malhotra S, Shah R. Women and mental health in India: An overview. Indian J Psychiatry. 2015; 57(Suppl 2):S205-11. [DOI:10.4103/0019-5545.161479] [PMID] [PMCID]
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960; 23(1):56-62. [DOI:10.1136/jnnp.23.1.56] [PMID] [PMCID]
Solmi F, Dykxhoorn J, Kirkbride JB. Urban-rural differences in major mental health conditions. In: Okkels N, Kristiansen CB, Munk-Jorgensen P, editors. Mental health and illness in the city. Singapore: Springer; 2016. [DOI:10.1007/978-981-10-0752-1_7-1]
Venkatesh BK, Thiralli J, Naveen MN, Kishorekumar KV, Arunachala U, Venkatasubramanian G, et al. Sex difference in age of onset of schizophrenia: findings from a community-based study in India. World Psychiatry. 2008; 7(3):173-6. [DOI:10.1002/j.2051-5545.2008.tb00191.x] [PMID] [PMCID]
Saunders JC. Families Living with severe mental illness: A literature review. Issues Ment Health Nurs. 2013; 24(2):175-98. [DOI:10.1080/01612840305301] [PMID]
Hosák L, Libiger J. Antiepileptic drugs in schizophrenia: A review. Eur Psychiatry. 2002; 17(7):371-8. [DOI:10.1016/S0924-9338(02)00696-X] [PMID]
Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: Overview and treatment options. P & T. 2014; 39(9):638-45. [PMID] [PMCID]
Zuo L, Luo X, Krystal JH, Cramer J, Charney DS, Gelernter J. The efficacies of clozapine and haloperidol in refractory schizophrenia are related to DTNBP1 variation. Pharmacogenet Genomic. 2009; 19(6):437-46. [DOI:10.1097/FPC.0b013e32832b9cfc] [PMID] [PMCID]
Dold M, Samara MT, Li C, Tardy M, Leucht S. Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders. Cochrane Database Syst Rev. 2015; 1:CD009831.[DOI:10.1002/14651858.CD009831.pub2] [PMID]
Moore TA, Buchanan RW, Buckley PF, Chiles JA, Conley RR, Crismon ML, et al. The Texas medication algorithm project antipsychotic algorithm for Schizophrenia. J Clin Psychiatry. 2007; 68(11):1751-62. [DOI:10.4088/JCP.v68n1115] [PMID]
Park KM, Kim SE, Lee BI. Antiepileptic drug therapy in patients with drug-resistant epilepsy. J Epilepsy Res. 2019; 9(1):14-26. [DOI:10.14581/jer.14003] [PMID] [PMCID]
Miller DD, Caroff SN, Davis SM, Rosenheck RA, McEvoy JP, Saltz BL, et al. Extrapyramidal side-effects of antipsychotics in a randomised trial. Br J Psychiatry. 2008; 193(4):279-88. [DOI:10.1192/bjp.bp.108.050088] [PMID] [PMCID]
Sykes DA, Moore H, Stott L, Holliday N, Javitch JA, Lane JR, et al. Extrapyramidal side effects of antipsychotics are linked to their association kinetics at dopamine D2 receptors. Nat Commun. 2017; 8(1):763. [DOI:10.1038/s41467-017-00716-z] [PMID] [PMCID]
Ogino S, Miyamoto S, Miyake N, Yamaguchi N. Benefits and limits of anticholinergic use in schizophrenia: Focusing on its effect on cognitive function. Psychiatry Clin Neurosci. 2014; 68(1):37-49. [DOI:10.1111/pcn.12088] [PMID]
Lader M, Petursson H. Rational use of anxiolytic/sedative drugs. Drugs. 1983; 25(5):514-28. [DOI:10.2165/00003495-198325050-00004] [PMID]
Pharmacotherapy is given to the patients according to the severity of the disease and associated complications. Pharmacotherapy involves drugs from different categories like antipsychotics, antidepressants, and anticonvulsants, and so on for treating different kinds of hallucinations, inducing schizophrenia (e.g. auditory, visual, olfactory, gustatory, etc.) [22]. For patients suffering from schizophrenia, the antipsychotic medication should be recommended as the first line of treatment. According to the American Psychiatric Association (APA), second-generation (atypical) Antipsychotics (SGAs) except clozapine are the agents of choice for the first-line treatment of schizophrenia. Clozapine is not recommended because of its risk of agranulocytosis [23]. Moreover, clozapine was found to be more effective than haloperidol for treating schizophrenia [24]. In our study, we observed that the first-generation antipsychotic agents are used almost twice more frequently than the second-generation agents in the treatment of schizophrenia in Bangladesh. Haloperidol is the most used first-generation agent. According to the 6-stage pharmacotherapeutic algorithm for the treatment of schizophrenia by the Texas Medication Algorithm Project (TMAP), stage 1 is the first-line monotherapy with an SGA. If the patient shows little or no response, he or she should proceed to the next stage which consists of monotherapy with either another SGA or First-Generation Antipsychotics (FGA). If there is still no response, the patient should move to stage 3, where clozapine monotherapy with monitoring of the White Blood Cell (WBC) count is suggested. If agranulocytosis arises, clozapine should be stopped. The patient should proceed to stage 4 in combination with clozapine and FGA or SGA, and or Electroconvulsive Therapy (ECT) if stage 3 therapy fails to give a positive response. If no treatment response is still observed from stage 4, monotherapy with an FGA or an SGA (that has not been tried) should be applied. Finally, stage 6 consists of combination therapy with an SGA, an FGA, ECT, and or a mood stabilizer if stage 5 treatment is unsuccessful [25-27]. We observed the use of the antiepileptic drug for some patients as a combination where the first three stages failed. No inconsistencies have been shown with the guidelines given by APA and TMAP.
It was observed that anticholinergic drugs, like procyclidine hydrochloride, are widely used in Bangladesh possibly to minimize the extrapyramidal side effects of antipsychotics. Anticholinergic drugs are being prescribed for symptomatic treatment of Parkinson disease for over a century and they are still trusted by physicians. For patients with psychosis and schizophrenia, anticholinergics are primarily used to counter the extrapyramidal side effects or prevent side effects induced by antipsychotics [28]. Extrapyramidal side effects such as Parkinsonism are believed to be the unavoidable result of antipsychotic efficacy conferred by dopamine D2 receptor blockade [29]. However, they can cause distressing peripheral side-effects (e.g. dry mouth and constipation) and CNS adverse effects (e.g. cognitive impairment, worsening of tardive dyskinesia, and delirium) [30].
We found that antidepressants were often prescribed to patients suffering from depression. Moreover, we observed that anxiolytics are prescribed to the patients suffering from debilitating anxiety to induce sedation. Benzodiazepines are the most widely prescribed anxiolytics in Bangladesh and are more effective than barbiturates and meprobamate [31]. Treatment with benzodiazepines may target a novel therapeutic mechanism beyond the scope of traditional antipsychotics. The present study has some limitations, for example, the severity of the disease, the duration of treatment, patient type (old or new), rate of antipsychotic combination therapy, and failure with previous treatment have not been reported.
We revealed the prescription pattern and demographic trend of schizophrenia in Bangladesh for the first time using large datasets. The study indicates antipsychotics and anticholinergics are the major drugs prescribed for treating schizophrenia. Besides, the first and second generations of antipsychotics are also prescribed in such a way that it complies with the authorized and established guidelines throughout the world. The present study findings will be helpful to physicians for treating schizophrenic patients.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the ethical review committee of the participating organizations. All investigations were performed according to the principles stated in the Declaration of Helsinki (Version 2008, Seoul, Korea).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and methodology: Zabun Nahar, Md. Rabiul Islam; Conduction, analysis, and initial draft writing: Salsabil Islam, Md. Sohan, Faysal Ahmed; Revise and editing of manuscript: Md. Rabiul Islam, Salsabil Islam, Md. Sohan; Supervision: Zabun Nahar, Md. Rabiul Islam; All authors reviewed and approved the final version of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We acknowledge the National Institute of Mental Health (NIMH), Dhaka, Bangladesh, and Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka Bangladesh for their administrative support, facilities, and instrumentations.
References
World Health Organization. Schizophrenia [Internet]. 2019 [Updated 4 October 2019]. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia
National Institute of Mental Health. Schizophrenia [Internet]. 2020 [Updated 10 May 2020]. Available from: https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml
Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. P & T. 2014; 39(9):638-45. [PMID] [PMCID]
Fountoulakis KN, Popovic D, Mosheva M, Siamouli M, Moutou K, Gonda X. Mood symptoms in stabilized patients with schizophrenia: A bipolar type with predominant psychotic featuews? Psychiatr Danub. 2017; 29(2):148-54.[DOI:10.24869/psyd.2017.148] [PMID]
Wu Y, Kang R, Yan Y, Gao K, Li Z, Jiang J, et al. Epidemiology of schizophrenia and risk factors of schizophrenia-associated aggression from 2011 to 2015. J Int Med Res. 2018; 46(10):4039-49. [DOI:10.1177/0300060518786634] [PMID] [PMCID]
McGrath J, Saha S, Chant D, Welham J. Schizophrenia: A concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008; 30:67-76. [DOI:10.1093/epirev/mxn001] [PMID]
Gejman PV, Sanders AR, Duan J. The role of genetics in the etiology of schizophrenia. Psychiatr Clin North Am. 2010; 33(1):35-66. [DOI:10.1016/j.psc.2009.12.003] [PMID] [PMCID]
Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: A meta-analysis of family high-risk studies. Schizophr Bull. 2013; 40(1):28-38. [DOI:10.1093/schbul/sbt114] [PMID] [PMCID]
Nishuty NL, Khandoker MMH, Karmoker JR, Ferdous S, Shahriar M, Qusar MMAS, et al. Evaluation of serum interleukin-6 and C-reactive protein levels in Drug-naïve major depressive disorder patients. Cureus. 2019; 11(1):e3868.. [DOI:10.7759/cureus.3868] [PMID] [PMCID]
Kim YK, Na KS, Myint AM, Leonard BE. The role of pro-inflammatory cytokines in neuroinflammation, neurogenesis and the neuroendocrine system in major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2016; 64:277-84. [DOI:10.1016/j.pnpbp.2015.06.008] [PMID]
Barbato A. Schizophrenia and public health [Internet]. 1998 [Updated 1998] Available from: https://www.who.int/mental_health/media/en/55.pdf
World Health Organization. WHO-aims report on mental health system in Bangladesh: A report of the assessment of the mental health system in Bangladesh using the World Health Organization - assessment instrument for mental health systems (WHO-AIMS) [Internet]. 2007 [Updated 2007]. Available from: https://www.who.int/mental_health/bangladesh_who_aims_report.pdf
Goetghebeur E. Book reviews: Lemeshow S, Homser DW Jr, Klar J, Lwanga SK 1990: Adequacy of sample size in health studies. Chichester: John Wiley & Sons for WHO. Stat Methods Med Res. 1992; 1(1):120. [DOI:10.1177/096228029200100108]
Didar Hossain M, Ahmed HََU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: A systematic review. BMC Psychiatry. 2014; 14:216. [DOI:10.1186/s12888-014-0216-9] [PMID] [PMCID]
Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of Schizophrenia. PLoS Med. 2005; 2(5):e141. [DOI:10.1371/journal.pmed.0020141] [PMID] [PMCID]
Hamza A, Sharma MK, Anand N, Marimuthu P, Thamilselvan P, Thakur PC, et al. Urban and rural pattern of Internet use among youth and its association with mood state. J Family Med Prim Care. 2019; 8(8):2602-6. [DOI:10.4103/jfmpc.jfmpc_428_19] [PMID] [PMCID]
Malhotra S, Shah R. Women and mental health in India: An overview. Indian J Psychiatry. 2015; 57(Suppl 2):S205-11. [DOI:10.4103/0019-5545.161479] [PMID] [PMCID]
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960; 23(1):56-62. [DOI:10.1136/jnnp.23.1.56] [PMID] [PMCID]
Solmi F, Dykxhoorn J, Kirkbride JB. Urban-rural differences in major mental health conditions. In: Okkels N, Kristiansen CB, Munk-Jorgensen P, editors. Mental health and illness in the city. Singapore: Springer; 2016. [DOI:10.1007/978-981-10-0752-1_7-1]
Venkatesh BK, Thiralli J, Naveen MN, Kishorekumar KV, Arunachala U, Venkatasubramanian G, et al. Sex difference in age of onset of schizophrenia: findings from a community-based study in India. World Psychiatry. 2008; 7(3):173-6. [DOI:10.1002/j.2051-5545.2008.tb00191.x] [PMID] [PMCID]
Saunders JC. Families Living with severe mental illness: A literature review. Issues Ment Health Nurs. 2013; 24(2):175-98. [DOI:10.1080/01612840305301] [PMID]
Hosák L, Libiger J. Antiepileptic drugs in schizophrenia: A review. Eur Psychiatry. 2002; 17(7):371-8. [DOI:10.1016/S0924-9338(02)00696-X] [PMID]
Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: Overview and treatment options. P & T. 2014; 39(9):638-45. [PMID] [PMCID]
Zuo L, Luo X, Krystal JH, Cramer J, Charney DS, Gelernter J. The efficacies of clozapine and haloperidol in refractory schizophrenia are related to DTNBP1 variation. Pharmacogenet Genomic. 2009; 19(6):437-46. [DOI:10.1097/FPC.0b013e32832b9cfc] [PMID] [PMCID]
Dold M, Samara MT, Li C, Tardy M, Leucht S. Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders. Cochrane Database Syst Rev. 2015; 1:CD009831.[DOI:10.1002/14651858.CD009831.pub2] [PMID]
Moore TA, Buchanan RW, Buckley PF, Chiles JA, Conley RR, Crismon ML, et al. The Texas medication algorithm project antipsychotic algorithm for Schizophrenia. J Clin Psychiatry. 2007; 68(11):1751-62. [DOI:10.4088/JCP.v68n1115] [PMID]
Park KM, Kim SE, Lee BI. Antiepileptic drug therapy in patients with drug-resistant epilepsy. J Epilepsy Res. 2019; 9(1):14-26. [DOI:10.14581/jer.14003] [PMID] [PMCID]
Miller DD, Caroff SN, Davis SM, Rosenheck RA, McEvoy JP, Saltz BL, et al. Extrapyramidal side-effects of antipsychotics in a randomised trial. Br J Psychiatry. 2008; 193(4):279-88. [DOI:10.1192/bjp.bp.108.050088] [PMID] [PMCID]
Sykes DA, Moore H, Stott L, Holliday N, Javitch JA, Lane JR, et al. Extrapyramidal side effects of antipsychotics are linked to their association kinetics at dopamine D2 receptors. Nat Commun. 2017; 8(1):763. [DOI:10.1038/s41467-017-00716-z] [PMID] [PMCID]
Ogino S, Miyamoto S, Miyake N, Yamaguchi N. Benefits and limits of anticholinergic use in schizophrenia: Focusing on its effect on cognitive function. Psychiatry Clin Neurosci. 2014; 68(1):37-49. [DOI:10.1111/pcn.12088] [PMID]
Lader M, Petursson H. Rational use of anxiolytic/sedative drugs. Drugs. 1983; 25(5):514-28. [DOI:10.2165/00003495-198325050-00004] [PMID]
Type of Study: Original Research |
Subject:
Rational Drug Prescribing
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |